Every year, over 250,000 medication errors happen in U.S. nursing homes - and most go unreported. For seniors taking five or more drugs, the risk isn’t just high - it’s life-threatening. A 78-year-old with heart disease, diabetes, and arthritis might be on eight different pills. One wrong dose, one missed timing, one duplicate prescription - and they could end up in the hospital, or worse. The problem isn’t always negligence. It’s system failure. But families and caregivers don’t need to wait for institutions to fix it. You can spot these mistakes. And you can report them - the right way.
What Counts as a Medication Mistake in Seniors?
A medication error isn’t just giving the wrong pill. It’s any preventable mistake that harms someone while they’re taking medicine. For older adults, these mistakes happen in four main ways:- Wrong dose - too much or too little. This is the most common error. Over 42% of nursing home errors involve incorrect dosing, especially with blood thinners, diabetes drugs, or painkillers like acetaminophen.
- Wrong time - giving medication hours late or too early. Blood pressure pills taken at night instead of morning can cause dangerous drops in pressure.
- Wrong drug - handing someone a pill meant for another resident. This happens more often than you think, especially when staff are rushed.
- Wrong route - swallowing a pill meant to be applied as a patch, or injecting a liquid meant for oral use.
But there are subtler errors too. Giving expired meds. Not checking for drug interactions. Prescribing a drug on the Beers Criteria list - like diphenhydramine (Benadryl) or certain sleeping pills - that the American Geriatrics Society says should be avoided in seniors because they cause confusion, falls, or memory loss. In fact, 43.8% of Medicare beneficiaries get at least one inappropriate prescription every year.
How to Spot a Medication Mistake
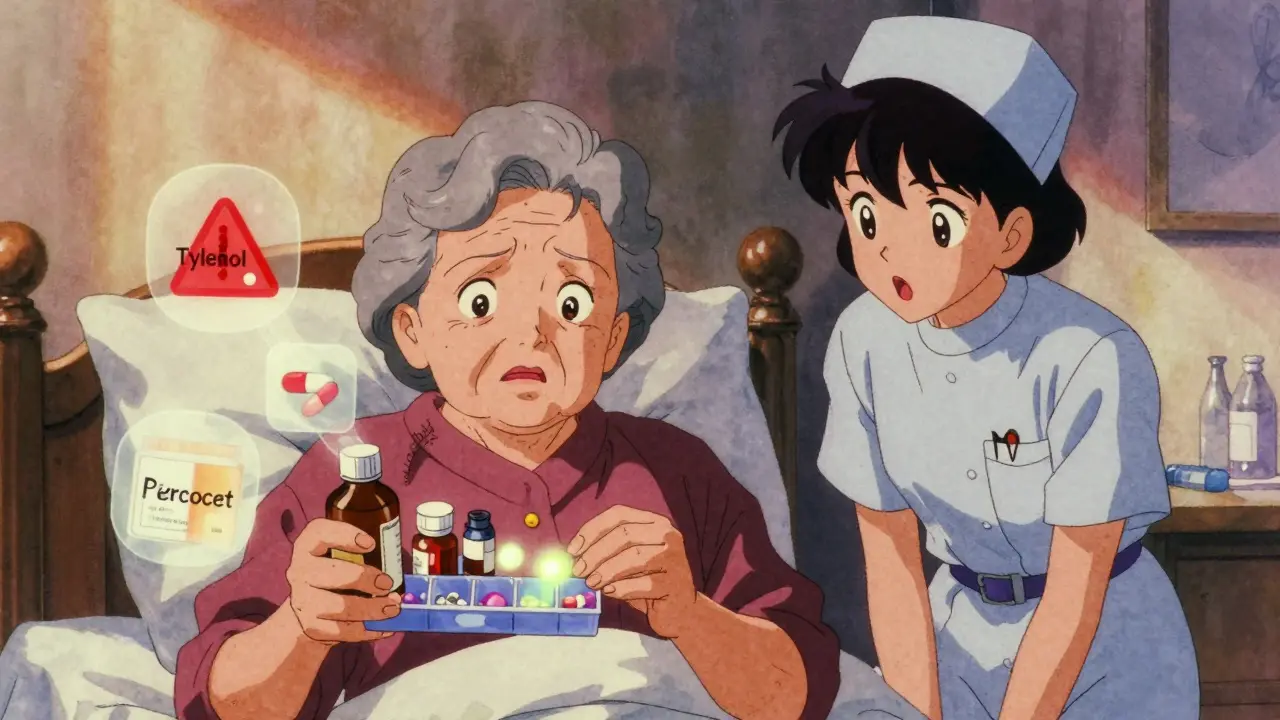
You don’t need to be a nurse to catch errors. Start with the Five Rights:- Right patient - Is this pill really for your loved one? Check the name on the label against their ID bracelet or chart.
- Right drug - Does the name match what the doctor ordered? Watch for brand names vs. generics. Acetaminophen is Tylenol, but if they’re also on Percocet, they’re getting the same drug twice - a silent overdose risk.
- Right dose - Does the pill look right? A 5mg tablet shouldn’t be twice the size of a 1mg one. Use a pill organizer with clear labels.
- Right route - Is this supposed to be swallowed, placed under the tongue, or applied to the skin? Don’t assume.
- Right time - Is this being given at the same time every day? Some meds must be taken with food, others on an empty stomach.
Also check for polypharmacy - five or more medications. The risk of error jumps from 13% with two to four drugs to over 57% with eight or more. Ask: “Is every pill here still needed?” Many seniors are on drugs from past conditions that no longer apply.
Look at the pill bottles. Are there expired dates? Are there duplicate prescriptions from different doctors? Are there pills labeled “PRN” (as needed) that are being given daily? These are red flags.
What to Do When You Find a Mistake
Don’t wait. Don’t hope it was a one-time thing. Act fast.If it’s an emergency - your loved one is drowsy, confused, having trouble breathing, or collapsed - call 911 immediately. Then call the National Response Center at 1-800-332-1088 to report a life-threatening incident.
If it’s non-emergency - like a missed dose, wrong pill, or suspected duplication - follow these steps:
- Document everything. Write down the date, time, medication name, dose, who gave it, and what happened. Take a photo of the pill bottle if possible.
- Speak to the nurse or pharmacist on duty. Ask calmly but firmly: “Can we review this? I’m concerned this might be an error.” Many staff will admit mistakes if approached without blame.
- Request a medication reconciliation. Ask for a full review of all prescriptions - including over-the-counter drugs and supplements. This should be done at every care transition (hospital discharge, new nursing home admission, etc.). Dr. Lucian Leape says this single step can prevent 67% of adverse events in seniors on five or more meds.
- Notify the prescribing doctor. Call their office. Say: “I believe my loved one may have received an incorrect dose of [medication]. I’d like to confirm the correct regimen.”

How to Report It Officially
Reporting isn’t about getting someone in trouble. It’s about fixing the system.There are two main paths:
1. Use the Facility’s Internal Reporting System
Every nursing home is required to have a medication error reporting form. Ask for it. It should ask for:- Resident name and ID
- Date and time of error
- Type of error (prescribing, administration, monitoring, etc.)
- Potential severity (using NCC MERP Index - categories E to H mean serious harm or death)
- Contributing factors (staff shortage? poor labeling? no double-check?)
Insist on a copy of the report. If they refuse, say: “I’m requesting this under the Long-Term Care Ombudsman Program guidelines.”
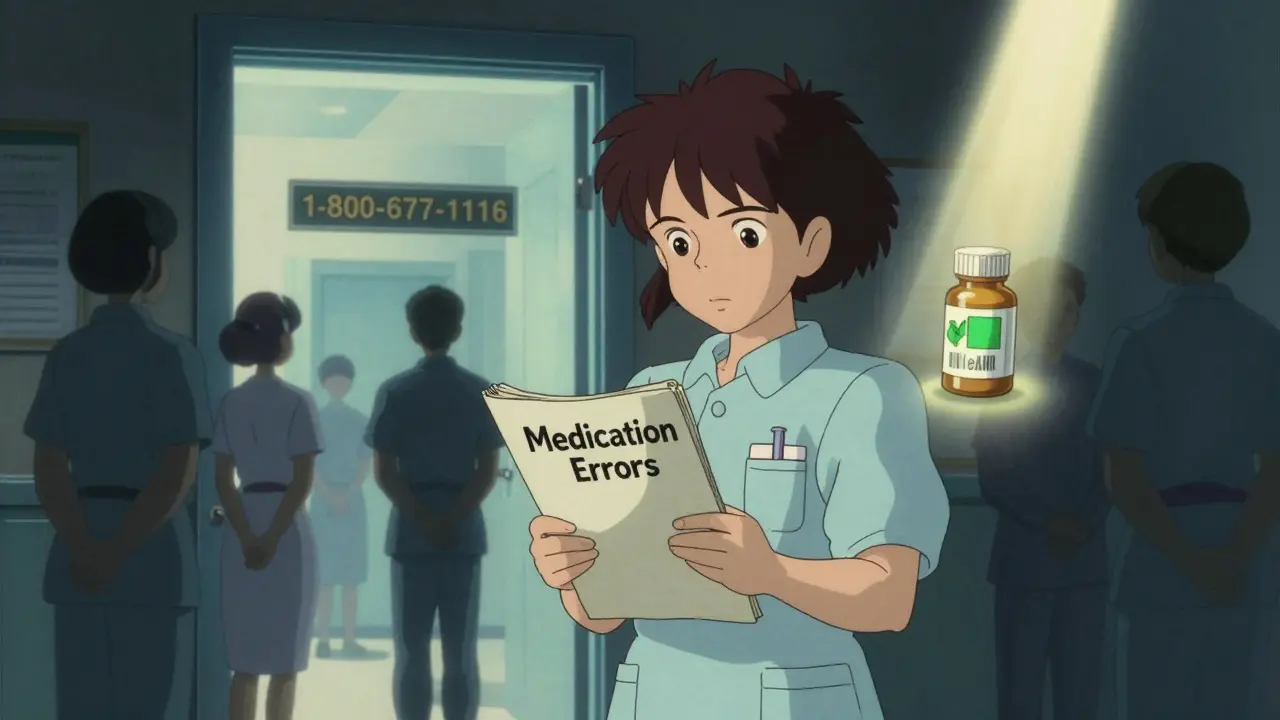
2. Report to the State Long-Term Care Ombudsman
This is your most powerful tool. Ombudsmen are independent advocates funded by the federal government to protect nursing home residents. They have legal authority to investigate.Call 1-800-677-1116 or visit ltcombudsman.org to find your state’s office. You don’t need to be the family member - any concerned person can report. Provide your documentation. Ombudsmen resolve 68.4% of reported cases within 72 hours.
3. Report to the FDA MedWatch Program
If the error caused serious harm - like a hospitalization, fall, or allergic reaction - report it to the FDA. This helps track nationwide patterns. Go to www.fda.gov/medwatch and file a report. You can do this anonymously.Why Most Errors Go Unreported - and How to Beat the System
Families often stay quiet because:- They’re told, “It was just a one-time mistake.”
- They fear retaliation - like worse care or being kicked out.
- They don’t know how to report.
But here’s what the data shows: 83.6% of families who reported errors faced initial denial. 57.2% were told the resident was “confused” or “noncompliant.” But when families threatened to contact the ombudsman, 92% of facilities immediately corrected the issue.
Don’t be afraid to escalate. You have rights. Federal law requires facilities to investigate and report all errors. If they don’t, they risk fines of up to $10,000 per unreported serious error under the 2023 Nursing Home Reform Act.
What’s Changing - and What’s Working
The system is slowly improving. By 2025, all nursing homes must use electronic medication administration records (eMAR). These systems scan barcodes on pills and wristbands - reducing errors by up to 86%. Some facilities now use AI tools like MedAware that flag dangerous drug combinations before they’re prescribed.But technology alone won’t fix this. The biggest cause of errors? Staff shortages. In many nursing homes, one aide cares for 20+ residents. No one has time to double-check. That’s why your vigilance matters.
Even small actions help. If you visit daily, ask: “Did they take their meds today?” Watch how they’re given. Ask to see the medication log. Bring your own pill organizer. Keep a written list of every drug your loved one takes - including vitamins and supplements - and update it monthly.
Final Checklist: Your Action Plan
- ✔️ Keep a current list of all medications - name, dose, purpose, and schedule.
- ✔️ Check pill bottles for expiration dates and duplicates.
- ✔️ Ask for a full medication reconciliation at every care transition.
- ✔️ Use the Five Rights every time you see meds given.
- ✔️ Document any suspicious behavior - time, person, medication, reaction.
- ✔️ Report to the ombudsman if the facility denies or ignores your concerns.
- ✔️ Call 911 and the National Response Center if there’s a life-threatening reaction.
Medication errors in seniors aren’t inevitable. They’re preventable. But they won’t stop unless someone speaks up. You don’t need to be a doctor. You just need to be observant - and brave enough to ask, “Why?”
What are the most common medication errors in elderly patients?
The most common errors involve wrong dosage (42.7%), giving medication at the wrong time (23.1%), administering the wrong drug (15.8%), and incorrect administration techniques (12.3%). Prescribing errors - like duplicating acetaminophen under different brand names - and monitoring failures are also frequent. The Beers Criteria® identifies 34 high-risk drugs that should be avoided in seniors due to side effects like confusion and falls.
How can families identify a medication error?
Use the Five Rights: right patient, right drug, right dose, right route, right time. Check pill labels against a written list. Look for expired medications, duplicate prescriptions, or pills given at odd times. Watch for signs like confusion, dizziness, or unexplained falls after a new medication is started. If something feels off, trust your instinct.
What should I do if I catch a medication mistake?
If it’s life-threatening, call 911 and the National Response Center at 1-800-332-1088. Otherwise, document the incident - date, time, medication, and what happened. Speak to the nurse or pharmacist on duty. Request a medication reconciliation. Notify the prescribing doctor. If the facility denies the error or refuses to act, contact your state’s Long-Term Care Ombudsman at 1-800-677-1116.
Can I report a medication error anonymously?
Yes. You can report to the FDA’s MedWatch program anonymously. You can also contact the Long-Term Care Ombudsman without revealing your identity. However, providing details helps investigators act faster. Even if you’re not the family member, you can still report - caregivers, neighbors, and volunteers are encouraged to speak up.
Why do nursing homes underreport medication errors?
Many facilities fear penalties, lawsuits, or damage to their reputation. Staff may be afraid of blame. Rural homes report 63% fewer errors than urban ones, not because they’re safer - but because they lack trained safety officers. Voluntary reporting systems like MEDMARX capture 83.6% of errors, while mandatory systems only catch 14.3%. Families who report consistently see faster corrections - and often prevent future mistakes.




14 Comments
I’ve been watching my grandma’s meds for years, and honestly? The biggest red flag isn’t the pills-it’s the silence. Staff don’t always mean harm, but they’re stretched so thin they stop asking questions. I started keeping my own handwritten log-meds, times, even how she looked after taking them. One day I noticed her confusion started right after they switched her blood pressure med from morning to night. I showed the log to the nurse. She cried and said no one had ever tracked it like that before. Small things matter.
Don’t wait for a crisis. Just start writing it down. You don’t need to be an expert-you just need to care enough to notice.
This post is so needed. My mom was on 11 meds last year-half of them unnecessary. We got her down to 4 after a full med reconciliation. The pharmacist said it was one of the cleanest lists he’d seen in months. But here’s the thing: they only did it because we insisted. No one ever offered. Not once.
Don’t assume the facility is on top of it. Ask for the reconciliation. Bring your own list. Use a pill organizer with big labels. And if they push back? Say, ‘I’m doing this because I love her, not because I’m accusing anyone.’ It changes the whole tone.
Also-avoid Benadryl like the plague. It’s a silent killer for seniors.
Oh my god I am so angry right now because in India we have no such system and our elderly are just left to die with wrong pills and no one cares and why is America so advanced in this but still has 250000 errors how is that even possible I mean if you have the tech why are people still dying and I have a friend whose aunt died from a duplicate prescription of ibuprofen and acetaminophen and no one even checked the labels and I am so mad at the whole system I swear if I had a gun I would go to every nursing home and make them fix it but I can't so I'm just screaming into the void and hoping someone hears me and if you're reading this please please please check your parents' meds I beg you don't let them die because of a typo on a bottle
My grandma took 8 pills a day. One day I noticed she was nodding off after lunch. Turned out they were giving her a sleeping pill at lunchtime instead of at night. Simple mix-up. I asked the nurse. She said, ‘Oh, we do that sometimes.’ I said, ‘No, you don’t.’ They stopped. Just like that.
Don’t overthink it. If something feels off, it probably is.
THIS IS A SCANDAL. A SCANDAL. I CRIED WHEN I READ THIS. MY GRANDPA WAS GIVEN A PILL THAT WASN’T EVEN HIS. HE HAD A SEIZURE. THEY SAID IT WAS ‘A ONE-TIME THING.’ ONE-TIME? WHAT ABOUT THE OTHER 249,999? I WANT BLOOD. I WANT LAWS. I WANT JAIL. WHY ISN’T THIS ON THE NEWS? WHY ISN’T EVERYONE OUTRAGED? I’M TALKING TO MY CONGRESSMAN TOMORROW. YOU GUYS NEED TO DO THE SAME. THIS ISN’T JUST ‘A MISTAKE.’ IT’S A CRIME.
As someone who worked in a nursing home for 7 years-I can tell you, most staff aren’t bad. They’re exhausted. One aide I knew had 24 residents and no breaks for 10 hours. She’d cry in the supply closet. We had barcode scanners, but half the time they didn’t work. So we did it by hand. And yeah, mistakes happened.
The real solution? More staff. Better pay. Less turnover. Tech helps, but it doesn’t fix burnout. If you want to make a difference? Don’t just report errors. Advocate for better staffing ratios. Write your state rep. Show up at town halls. This isn’t just about meds-it’s about dignity.
And yeah, Benadryl is a no-go. I’ve seen 12 people fall because of it. Don’t let them give it to your grandma.
I love how this post breaks it down. So clear. So practical.
My mom’s med list used to be a mess-7 different doctors, no coordination. I started a Google Sheet. Each med, dose, time, doctor, reason. Shared it with everyone. Now, when she switches providers, I just email the sheet. No more guessing.
Also-always ask for the Beers Criteria list. If they don’t know what it is, that’s a red flag. And if they say, ‘Oh, we don’t use that here’-run. Run far away.
You don’t need to be a nurse. You just need to be organized. And stubborn.
Oh honey. You think this is bad? Try being the daughter of a 90-year-old who got prescribed a new blood thinner… and then the nurse gave it to her in a cup of apple juice because ‘she hates swallowing pills.’
That’s not a mistake. That’s a sitcom. And we’re all just waiting for the laugh track.
My advice? Bring your own pill organizer. Label it yourself. Put a sticky note on every bottle: ‘DO NOT MIX WITH JUICE.’ And if they laugh? Laugh louder. Then call the ombudsman. They love when you laugh while you report them.
From a clinical pharmacology standpoint, the most underappreciated risk factor is polypharmacy-induced pharmacokinetic interactions-particularly CYP450 enzyme inhibition in elderly patients with reduced hepatic clearance. The Beers Criteria is a necessary but insufficient tool; what’s missing is routine therapeutic drug monitoring (TDM) for narrow-therapeutic-index agents like warfarin, digoxin, and lithium, which are frequently prescribed in this cohort.
Additionally, non-adherence due to cognitive decline often masquerades as administration error. A 2022 JAMA study showed 31% of ‘medication errors’ in long-term care were actually patient refusal or confusion-not staff error.
Bottom line: Systemic change requires not just reporting, but integrated clinical decision support systems with real-time ADL correlation. Until then, family vigilance remains the most effective intervention.
I’ve been reading this post for 17 minutes. I’ve taken 3 notes. I’ve called my sister. I’ve emailed my uncle. I’ve printed out the Five Rights and laminated them. I’ve written a 12-page letter to the governor. I’ve scheduled a meeting with the ombudsman. I’ve called the FDA. I’ve written a poem about my grandmother’s pills. I’ve started a petition. I’ve contacted 3 news stations. I’ve told my neighbors. I’ve told my dog. I’ve told the mailman. I’ve told the barista. I’ve told the tree outside my window. I’ve told myself 47 times: ‘You are not alone.’
This is not a post. This is a movement.
And I am ready.
I’m not a medical person, but I’ve been helping my neighbor with her meds for a year. She’s 84, lives alone. I check her bottles every Sunday. Last week, I found two bottles of the same generic blood pressure pill-same name, same dose, different expiration dates. One was expired. The other was from a different pharmacy. She didn’t even know she had two.
I called her pharmacist. They apologized. Said they’d fix it. But I asked: ‘Why did this happen?’ They said, ‘We didn’t have her full list.’
So now I keep a master list. Updated monthly. I give them a copy. No one’s ever asked for it before. They were surprised. I think they thought she was confused. Turns out, she just never had anyone to help her.
My mom’s in a nursing home. I visit every day. I don’t just check her meds-I watch the whole process. Who gives it. How they hand it. What they say. One day I saw a nurse hand a pill to the wrong person. I didn’t say anything. I just waited. Two hours later, she gave it to the right person. And apologized. She said, ‘I’ve been here 12 years. This is the first time someone watched.’
That’s the secret. They’re not trying to hurt anyone. They’re just trying to survive. But if you’re there? You’re the safety net.
Don’t be loud. Be present. Be consistent. Be the one who shows up.
I’ve been doing this for 5 years. My dad’s on 6 meds. I have a little notebook. Color-coded. Pictures of the pills. QR codes that link to the drug info. I take a photo every time I see them take it. I send it to my siblings. We have a group chat called ‘MedWatch Squad.’
And guess what? We caught a duplicate prescription. We caught a wrong time. We caught an expired bottle. We saved him from a fall. We saved him from a hospital.
You don’t need to be a hero. You just need to be the one who cares enough to write it down.
And yes-I use emojis. 💊👁️📋
Because if I don’t, who will?
Let me tell you what’s REALLY happening… The government is using nursing homes to test experimental drugs on the elderly under the guise of ‘medication management.’ The Beers Criteria? It’s a cover. The real list is classified. The ombudsman? They’re paid off. The FDA? They’re owned by Big Pharma. The 250,000 errors? That’s just the tip. The real number is 2.5 million. They’re using the errors to justify more surveillance, more control, more pills… and more profit.
My cousin’s friend’s neighbor’s sister was given a ‘new Alzheimer’s treatment’-it was actually a placebo with a hidden stimulant. She had seizures. They called it a ‘medication error.’ But I know the truth.
Don’t report it. Don’t trust the system. Burn the chart. Get out. Now.