
Treatment Choice Advisor
Find the right treatment for your condition
Select your situation to see which treatments might be most appropriate. Based on the latest research and clinical guidelines.
Recommended Treatments
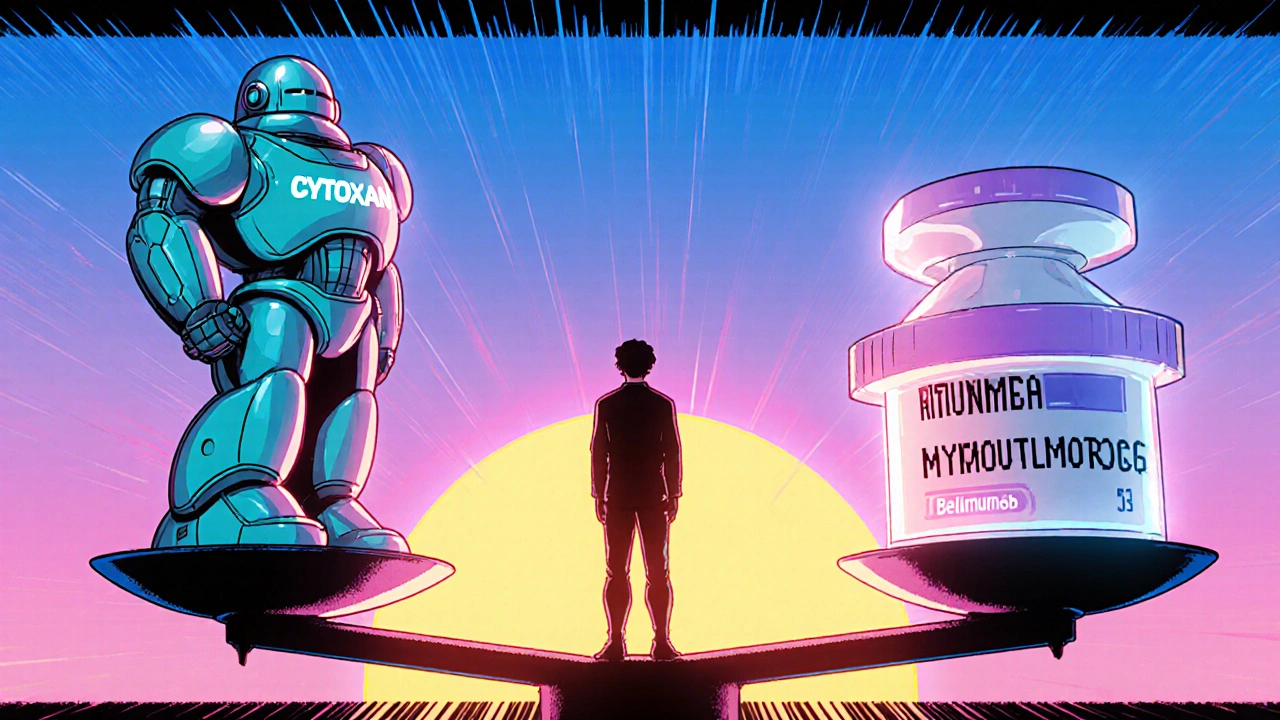
Cytoxan (cyclophosphamide) has been a backbone of cancer and autoimmune disease treatment for over 60 years. But it’s not the only option anymore. Today, doctors regularly weigh Cytoxan against newer drugs that may offer similar results with fewer side effects. If you’re facing treatment for lymphoma, leukemia, lupus, or vasculitis, knowing how Cytoxan stacks up against alternatives can help you ask better questions and make more informed choices.
How Cytoxan Works and When It’s Used
Cytoxan is an alkylating agent - a type of chemotherapy that damages the DNA inside fast-growing cells. That’s why it’s effective against cancer cells, which multiply quickly. But it doesn’t stop there. It also hits immune cells, which is why it’s used for autoimmune diseases like lupus nephritis, granulomatosis with polyangiitis, and severe rheumatoid arthritis.
It’s given either orally as a pill or through IV infusion. Dosing depends on the condition, weight, and kidney function. For lymphoma, doses are high and given in cycles. For autoimmune conditions, lower doses are used long-term to suppress the immune system without killing off too many healthy cells.
But here’s the catch: Cytoxan doesn’t just target bad cells. It can wreck healthy ones too. Common side effects include nausea, hair loss, low blood counts, and bladder irritation. Long-term use raises the risk of bladder cancer and infertility. That’s why many patients and doctors now look at alternatives.
Alternative 1: Rituximab (Rituxan)
Rituximab is a monoclonal antibody that targets CD20, a protein found on B-cells - the immune cells that go haywire in many autoimmune diseases. Unlike Cytoxan, which broadly suppresses the immune system, Rituximab is more precise. It doesn’t touch T-cells or other immune components.
In lupus nephritis, clinical trials show Rituximab works just as well as Cytoxan at reducing kidney inflammation. The New England Journal of Medicine published a 2010 study where 50% of patients on Rituximab achieved remission after 6 months - similar to Cytoxan’s 53%. But side effects were milder: less hair loss, no increased bladder cancer risk, and fewer infections.
It’s now a first-line option for many patients with ANCA-associated vasculitis. It’s given as IV infusions every 2 weeks for 6 months, then as needed. Costs are higher - about $10,000 per infusion - but fewer hospital visits for side effect management often balance it out.
Alternative 2: Mycophenolate Mofetil (CellCept)
Myophenolate mofetil blocks the production of DNA in lymphocytes, slowing down the immune response. It’s widely used in organ transplant patients and has become a go-to for lupus nephritis.
A 2017 study in Lancet compared Mycophenolate with Cytoxan in 500 patients with lupus nephritis. After 3 years, both groups had similar remission rates. But Mycophenolate had fewer serious infections, less hair loss, and no increased risk of leukemia. It’s taken as two pills a day, making it easier to manage than IV treatments.
It’s not perfect. Diarrhea and stomach upset are common early on. It also requires regular blood tests to monitor white blood cell counts. But for many, especially women planning pregnancy, it’s a safer bet than Cytoxan, which can cause birth defects.
Alternative 3: Azathioprine (Imuran)
Azathioprine has been around since the 1960s and is one of the oldest immunosuppressants. It’s a prodrug that breaks down into 6-mercaptopurine, which interferes with DNA synthesis in immune cells.
It’s often used after Cytoxan to maintain remission in autoimmune diseases. For example, if a patient gets their lupus under control with Cytoxan, doctors switch them to azathioprine for long-term control. It’s cheaper - under $50 a month - and taken as a daily pill.
But it’s slower to work. It can take 3 to 6 months to see full effects. It also carries a risk of liver toxicity and low white blood cell counts. Some patients have a genetic variation (TPMT deficiency) that makes them extremely sensitive to it, leading to dangerous drops in blood cells. Testing for this gene is now standard before starting.
It’s not as strong as Cytoxan for severe flares, but it’s a solid maintenance option with a long safety track record.
Alternative 4: Cyclosporine and Tacrolimus
These are calcineurin inhibitors - they block a specific signal that T-cells need to activate. They’re used mostly in kidney diseases like nephrotic syndrome and sometimes in lupus.
Cyclosporine can be very effective for steroid-resistant nephrotic syndrome in children. Tacrolimus, a stronger version, is often used in kidney transplant patients and now in lupus nephritis when other drugs fail.
Both require careful blood level monitoring. Side effects include high blood pressure, kidney damage over time, tremors, and gum overgrowth. They’re not first-line for most autoimmune conditions, but they’re valuable when other options don’t work or aren’t tolerated.
Alternative 5: Belimumab (Benlysta)
Belimumab is the first drug approved specifically for lupus. It targets BLyS, a protein that helps B-cells survive. By blocking BLyS, it reduces the number of abnormal B-cells driving lupus flares.
It’s not a replacement for Cytoxan in severe organ-threatening disease. But for moderate lupus with skin and joint involvement, it’s a game-changer. A 2011 FDA trial showed 43% of patients on Belimumab had fewer flares compared to 34% on placebo.
It’s given as a monthly IV infusion or weekly subcutaneous injection. Side effects are mild: headaches, nausea, and occasional infections. It doesn’t cause hair loss or bladder damage. But it’s expensive - over $30,000 a year - and only approved for active, autoantibody-positive lupus.
Choosing the Right Option
There’s no single best drug. The right choice depends on:
- What condition you have: Cytoxan is still top for aggressive lymphoma. Rituximab leads for ANCA vasculitis. Mycophenolate is preferred for lupus nephritis in women of childbearing age.
- Your age and fertility plans: Cytoxan can cause permanent infertility. Alternatives like Rituximab or Belimumab don’t carry that risk.
- Your kidney and liver health: Azathioprine and cyclosporine need organ monitoring. Rituximab is gentler on the liver.
- Cost and access: Generic Cytoxan costs less than $100 a month. Newer drugs can cost thousands. Insurance coverage varies widely.
- How fast you need results: Cytoxan works in weeks. Azathioprine takes months.
Many patients start with Cytoxan for a short burst to get control, then switch to a maintenance drug like Mycophenolate or Azathioprine. Others skip Cytoxan entirely if their disease isn’t life-threatening.
What About Newer Drugs Like Ibrutinib or CAR-T?
In lymphoma, newer targeted drugs like ibrutinib (a BTK inhibitor) and CAR-T cell therapy are replacing Cytoxan in relapsed cases. CAR-T, which reprograms a patient’s own immune cells to hunt cancer, has shown over 80% response rates in some aggressive lymphomas - far better than Cytoxan’s 30-40%.
But these are reserved for advanced or treatment-resistant disease. They’re complex, expensive, and require specialized centers. For most patients, Cytoxan and its alternatives remain the standard.
Real-World Trade-offs
One 58-year-old woman with lupus nephritis switched from Cytoxan to Mycophenolate after two cycles. Her hair grew back, her nausea disappeared, and she avoided a cystoscopy to check for bladder damage. She’s been in remission for 4 years.
Another patient, a 42-year-old man with ANCA vasculitis, got Rituximab instead of Cytoxan. He had two infusions and went into remission. No hair loss. No bladder issues. He’s now on maintenance azathioprine.
These aren’t rare stories. More doctors are starting with alternatives - especially when the goal is long-term control, not just quick damage control.
When Cytoxan Still Makes Sense
Cytoxan isn’t outdated. It’s still the most effective drug for:
- High-grade lymphomas and leukemias
- Severe, life-threatening vasculitis
- Patients who can’t afford expensive biologics
- Those who haven’t responded to other immunosuppressants
It’s also the most studied. We know its long-term risks better than any newer drug. That matters when you’re treating a 20-year-old who might live another 60 years.
For many, Cytoxan is the tool that saves their life - even if it comes with heavy baggage. The goal isn’t to eliminate it. It’s to use it wisely, and only when needed.
Is Cytoxan still used today, or is it outdated?
Yes, Cytoxan is still widely used, especially for aggressive cancers like lymphoma and leukemia, and for severe autoimmune diseases like vasculitis. While newer drugs are replacing it in some cases, it remains a first-line option where rapid, strong immune suppression is needed. Its low cost and long track record keep it in use.
Which alternative to Cytoxan has the fewest side effects?
Belimumab and Rituximab generally have fewer severe side effects than Cytoxan. They don’t cause hair loss, bladder damage, or infertility. Belimumab is the mildest, with mostly mild nausea and headaches. Rituximab can cause infusion reactions but doesn’t damage organs long-term. Mycophenolate is also gentler than Cytoxan, though it can cause stomach upset.
Can I avoid Cytoxan if I want to have children?
Yes. Cytoxan can cause permanent infertility in both men and women, especially with high or repeated doses. Alternatives like Rituximab, Belimumab, and Mycophenolate don’t carry this risk. If you’re planning pregnancy, your doctor will likely avoid Cytoxan and choose one of these instead.
How do I know if my insurance will cover an alternative to Cytoxan?
Insurance often requires step therapy - meaning you must try cheaper drugs like azathioprine or Mycophenolate first. Biologics like Rituximab and Belimumab usually need prior authorization. Ask your doctor to submit a letter explaining why Cytoxan isn’t right for you. Many patients successfully appeal denials with medical documentation.
Are there natural alternatives to Cytoxan?
No. There are no proven natural alternatives that can replace Cytoxan for cancer or serious autoimmune diseases. Supplements like turmeric or omega-3s may help reduce inflammation, but they won’t stop cancer or control vasculitis. Relying on them instead of prescribed drugs can be dangerous. Always discuss supplements with your doctor - they can interfere with treatment.
If you’re considering switching from Cytoxan, talk to your rheumatologist or oncologist about your goals: remission, quality of life, fertility, or cost. The best treatment isn’t always the newest - it’s the one that works for you, without breaking you.





14 Comments
Just had my third Rituximab infusion last week - no hair loss, no nausea, and I actually slept through the night for once. Still waiting on the biopsy results, but fingers crossed this is the switch that finally gives me back my life.
My doctor just told me to switch from Cytoxan to CellCept... guess I’m lucky I didn’t get bladder cancer first 😅
It is not merely a matter of cost or convenience - it is a question of survival. Cytoxan remains the most potent agent we have for aggressive lymphoma. To dismiss it as outdated is not only irresponsible, it is dangerous. The data does not lie.
Let’s be real - Cytoxan is the old-school hammer. It works, sure, but it also smashes your kneecaps, your ovaries, and your will to live. Meanwhile, Rituximab is like a precision scalpel - cuts out the bad cells, leaves your hair, your bladder, and your dignity intact. Why would anyone start with the hammer unless they’re out of options? Or money? Or both?
I’m curious how many of these "alternatives" are just pharma’s way of selling the same thing at 100x the price. Azathioprine’s been around since Nixon was president and still works fine. Why do we need a $30K/year drug just to avoid a little nausea? Someone’s getting rich here, and it ain’t the patient.
It is fascinating to observe the cultural divergence in treatment paradigms. In the United States, cost and innovation drive decision-making. In contrast, European systems often prioritize long-term safety and cost-effectiveness, leading to greater adoption of azathioprine and mycophenolate. This raises the question: are we treating disease, or managing healthcare economics?
My sister went from Cytoxan to Belimumab after her third flare. She cried when her hair started growing back. Not because she’s vain - because she finally felt like herself again. This isn’t just medicine. It’s identity. And if we can give someone back their identity without destroying their body? That’s not a replacement. That’s progress.
Look, I’ve been on Cytoxan for lupus for five years. I’ve had cystoscopies, I’ve lost my fertility, I’ve spent nights vomiting while my kids slept next door. I switched to Rituximab last year. I’ve had one infusion since. No side effects. No hospital stays. No nightmares. I’m not mad at Cytoxan - it saved my life. But I’m damn glad I didn’t have to keep living with it. The future isn’t about replacing the old - it’s about giving people a reason to want to live beyond surviving.
Everyone’s acting like these "alternatives" are some kind of miracle. They’re not. They’re just slower, more expensive, and less proven over decades. You trade one set of risks for another - maybe less bladder cancer, but more opportunistic infections, or worse, no effect at all. The truth? There’s no magic bullet. There’s only trade-offs. And most patients don’t get to choose - insurance does.
So... we're just supposed to believe that a $30k/year drug is "better" because it doesn't make you lose your hair? Cool. I'll just keep my hair and my cancer. 🙃
I am from India, and here, Cytoxan is still the most accessible option for low-income patients. My cousin with vasculitis was prescribed it because Rituximab costs more than our annual household income. We cannot afford the "better" options - but we are still alive. This is not a luxury debate. It is a matter of survival.
Let’s stop pretending this is about patient care. This is about patent expiration. Pharma wants to kill Cytoxan because it’s generic. They’re pushing biologics like they’re the only real medicine. But the truth? Cytoxan still works better in 70% of severe cases. The rest of you are just drinking the Kool-Aid because your doctor got a free trip to Orlando.
I’ve read through all of this, and honestly? I feel like we’re missing the human part. It’s not just about side effects or costs or even efficacy. It’s about dignity. One person gets to keep their hair. Another gets to plan a family. Someone else gets to wake up without dreading the nausea. These aren’t just medical choices - they’re choices about who you get to be while you’re still alive. That matters more than any trial data.
I’m a nurse in oncology. I’ve seen patients cry because they lost their hair on Cytoxan. I’ve seen others sob because they couldn’t have kids after it. And I’ve seen the same people light up when they get Rituximab - not because it’s "new," but because they finally feel like they’re not being punished for being sick. This isn’t just science. It’s humanity. And we’re finally starting to see it.