
Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication errors. Many of these mistakes aren’t caused by doctors or pharmacists-they happen at home, when someone takes the wrong pill, at the wrong time, or in the wrong way. You might think you’re doing everything right, but small oversights can lead to big problems. The good news? Most of these errors are preventable. There are five essential rules that form the foundation of safe medication use-whether you’re taking one pill a day or managing a dozen. These aren’t just hospital protocols; they’re practical steps anyone can follow to protect their health.
Rule 1: Know Exactly What You’re Taking
It sounds simple, but many people don’t actually know the name of their medication. They might call it "the blue pill" or "the one for my blood pressure," but that’s not enough. You need to know both the brand name and the generic name. For example, if you’re taking metoprolol, don’t just remember "the heart pill." Know that it’s also sold as Toprol-XL. Look-alike, sound-alike drugs are a major cause of errors. Insulin and heparin, for instance, are often confused because their packaging looks similar. The Institute for Safe Medication Practices says these mix-ups cause about 25% of reported medication errors. Always check the label when you pick up a prescription. Compare the pill’s color, shape, and imprint to what you’ve taken before. If something looks different, ask your pharmacist. Don’t assume it’s just a new batch. A change in appearance could mean a different drug entirely.Rule 2: Take the Right Dose
Dosing mistakes are one of the most common and dangerous errors. A milligram (mg) isn’t the same as a microgram (mcg)-and mixing them up can be deadly. This is especially true for children, older adults, and people with kidney or liver problems. Insulin, blood thinners like warfarin, and opioids are high-alert medications where even a small mistake can cause serious harm. Always double-check the dose on the prescription label. If your doctor says "take 5 mg," make sure the bottle says the same thing. Use a proper measuring tool-never a kitchen spoon. A teaspoon holds about 5 mL, but a tablespoon holds 15 mL. That’s three times too much. If you’re taking multiple medications, keep a written list that includes the dose, frequency, and reason for each one. Update it every time something changes. Many people don’t realize that some medications need to be taken with food, others on an empty stomach. Getting this wrong can make the drug less effective-or more toxic.Rule 3: Take It at the Right Time
Timing matters more than most people think. Some medications need to be taken exactly every 12 or 24 hours to stay effective. Blood pressure pills, antibiotics, and anticoagulants are time-sensitive. If you take your blood thinner too early or too late, your risk of clotting or bleeding changes. The standard window for most medications is 30 minutes before or after the scheduled time. But for some, like certain antibiotics or chemotherapy pills, the window is as tight as 15 minutes. A 2022 Kaiser Family Foundation survey found that 61% of adults over 65 had at least one time-related mistake in the past year. They skipped doses, doubled up, or took pills at random times because they forgot or got confused. Use a pill organizer with compartments for morning, afternoon, evening, and night. Set phone alarms. Don’t rely on memory. If you miss a dose, check the label or call your pharmacist. Don’t just take two pills to make up for it-that’s how overdoses happen.
Rule 4: Use the Correct Route
This means taking the medicine the way it was meant to be taken. Oral pills shouldn’t be crushed unless the label says it’s safe. Some extended-release tablets will release the full dose at once if crushed, leading to overdose. Injectable medications should never be taken by mouth. A 2021 AHRQ study found that 16% of medication errors involved the wrong route. One case involved a patient who was given a cream meant for skin use-inside their eye. Another involved a child who swallowed a patch meant to be worn on the skin. Always read the instructions. If your medication comes as a liquid, use the dropper or syringe that came with it. If it’s a nasal spray, don’t swallow it. If it’s a suppository, don’t try to take it orally. And never assume a pill can be dissolved in water or juice unless your pharmacist confirms it’s safe. Some medications break down in stomach acid and lose their effect.Rule 5: Confirm It’s Really You
This rule isn’t just for hospitals. Even at home, you need to make sure the medication is meant for you. People often share pills-"I have the same headache, just take mine." That’s dangerous. A drug that works for someone else might interact with your other medications, cause an allergic reaction, or be the wrong dose for your body. Even if you’re both taking the same drug, your dosing could be different based on weight, age, or kidney function. Always check the name on the prescription bottle. If you’re picking up medication at the pharmacy, confirm your full name and date of birth. Never let someone else pick up your prescriptions unless you’ve given them written permission. If you live with others, store your medications separately. Use locked boxes or cabinets. A 2023 ISMP report showed that 22% of patients who followed label directions still had harm because they took someone else’s medicine by accident.What’s Missing? The Other Things You Should Know
The five rules above are the core, but safety goes deeper. Always ask: "Why am I taking this?" and "What side effects should I watch for?" Many people don’t realize that some medications can make you dizzy, sleepy, or prone to falls. If you’re on five or more drugs, ask your doctor or pharmacist for a medication review every six months. Polypharmacy-the use of multiple medications-is the biggest risk factor for errors in older adults. Keep a current list of everything you take, including vitamins, supplements, and over-the-counter drugs. Bring this list to every appointment. Also, check expiration dates. Old medications can lose potency or even become harmful. Don’t store pills in the bathroom-heat and moisture ruin them. Keep them in a cool, dry place. And if you ever feel something’s off-dizziness, rash, nausea, confusion-stop taking the drug and call your provider. Don’t wait.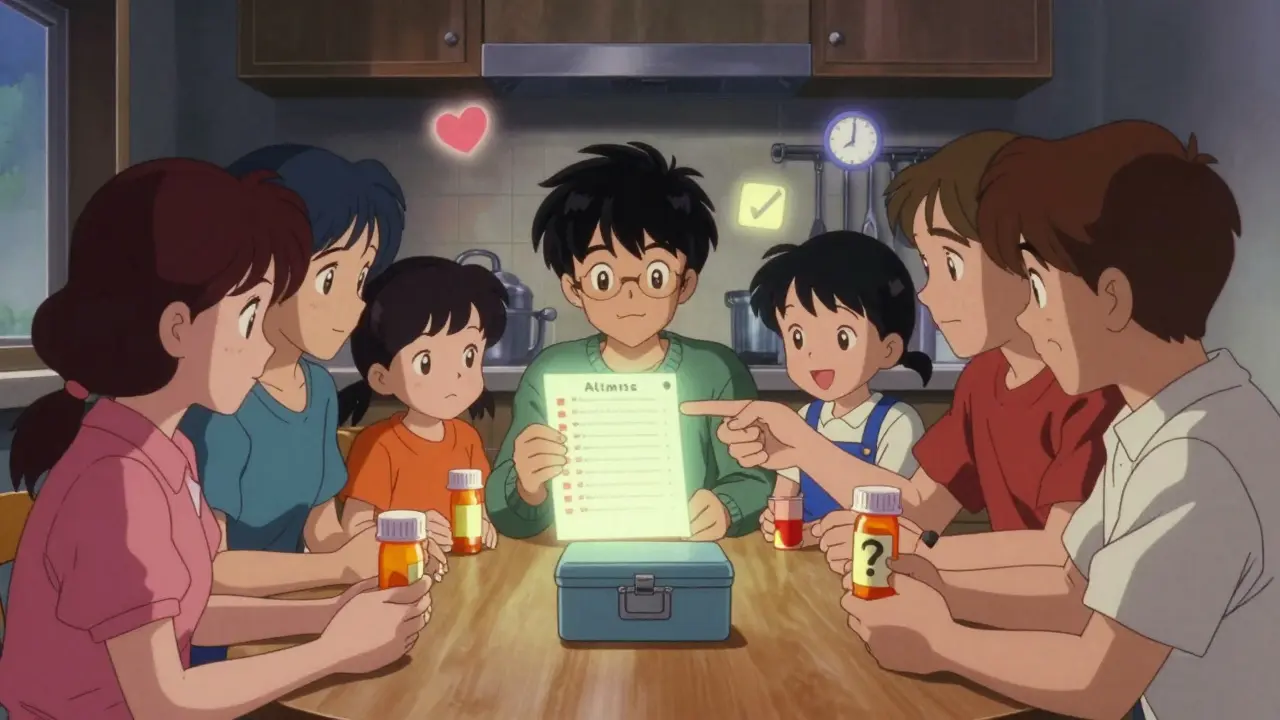
Tools That Help
You don’t have to rely on memory alone. Pill organizers with alarms are widely available and cost under $20. Smartphone apps like Medisafe or MyTherapy can send reminders and track your doses. Many pharmacies offer free blister packs pre-filled by week. If you’re on complex meds, ask your pharmacist about a "brown bag review"-bring all your bottles to your appointment and let them check for interactions. Some pharmacies now use barcode scanning to match your prescription to your profile, reducing errors at the counter. For seniors, community health centers often offer free medication management programs. Don’t hesitate to ask for help. You’re not alone-45% of adults need extra tools to manage their meds safely.Final Thought: Safety Is a Habit, Not a One-Time Check
Medication safety isn’t something you do once when you get your prescription. It’s a daily habit. It’s checking the label every time. It’s asking questions when something doesn’t look right. It’s writing things down and keeping your list updated. The five rules aren’t just guidelines-they’re lifelines. They’ve been proven to reduce errors by up to 56% when followed consistently. Even small actions-like using the right measuring tool or confirming your name on the bottle-can prevent hospital visits, serious injury, or worse. You’re the last line of defense. Be the one who catches the mistake before it happens.What should I do if I accidentally take the wrong medication?
Don’t panic, but act quickly. Call your pharmacist or poison control center immediately (1-800-222-1222 in the U.S.). Do not wait for symptoms to appear. Have the medication bottle with you when you call so you can give details about the name, dose, and time taken. If you’re having trouble breathing, chest pain, or severe dizziness, call 911. Never try to induce vomiting unless instructed by a professional.
Can I split my pills to save money?
Only if the pill has a score line and your doctor or pharmacist says it’s safe. Extended-release, enteric-coated, or capsule-form pills should never be split. Splitting them can release the full dose at once, causing overdose. Even pills that look safe to split can be uneven, leading to inconsistent dosing. Ask your pharmacist if a lower-strength tablet is available instead.
Why do some medications need to be taken with food and others on an empty stomach?
Food can change how your body absorbs the drug. Some medications need food to reduce stomach upset, like antibiotics such as amoxicillin. Others, like thyroid medicine or certain cholesterol drugs, must be taken on an empty stomach because food blocks absorption. Always follow the label instructions. If you’re unsure, ask your pharmacist to explain why the timing matters.
Is it safe to take expired medications?
Most expired medications lose potency over time, meaning they may not work as well. Some, like insulin or liquid antibiotics, can become harmful. The FDA advises against using expired drugs, especially for serious conditions. If you’re unsure, take the bottle to your pharmacy-they’ll dispose of it safely. Never keep old prescriptions just in case. They’re not a substitute for a current prescription.
How can I avoid mixing up my medications if I take a lot?
Use a pill organizer labeled with days and times. Keep a written list updated with names, doses, and times. Take a photo of your pill bottles and save it on your phone. Ask your pharmacist for a color-coded system or blister packs. Schedule a monthly "med check" with a family member or friend to review what you’re taking. Never rely on bottle shapes or colors-they change.





15 Comments
Man, I never realized how many ways you can screw up a pill. I used to just grab whatever looked like my usual blue one and call it a day. Now I keep a little notebook by my meds cabinet. Even wrote down the damn imprint codes. My grandma would be proud.
Rule 5 saved my life last year. My neighbor gave me his leftover painkillers after I mentioned my back was acting up. I took one. Two hours later, I was sweating bullets and dizzy as hell. Turned out it was a high-dose opioid he used for cancer pain. I called poison control. They told me to go to the ER. I didn’t argue.
So let me get this straight - we’re supposed to trust Big Pharma’s pill colors and shapes? LOL. My cousin got the same generic blood pressure med for six months, then one day it was a pink oval instead of a white oblong. She took it. Ended up in the hospital with a BP of 210/130. The pharmacy said it was "just a different manufacturer." Meanwhile, the FDA’s been quietly letting these swaps slide for years. Coincidence? I think not.
Rule 1 is meaningless without understanding pharmacokinetics. You can know the generic name all day, but if you don’t understand CYP450 metabolism, you’re just memorizing labels like a parrot. Metoprolol’s half-life is 3-7 hours depending on your CYP2D6 genotype. If you’re a poor metabolizer, Toprol-XL could accumulate to toxic levels. Most people don’t even know what CYP stands for. This article is a glorified pamphlet.
Thank you for this comprehensive guide. I work as a clinical pharmacist and can confirm: adherence to these five rules reduces medication-related hospitalizations by over 50% in elderly populations. The most common error remains dose confusion - particularly with insulin and anticoagulants. I encourage every patient to maintain a printed, color-coded medication list and update it after every provider visit. Consistency is non-negotiable.
I started using Medisafe last month and it’s a game-changer. I have 8 meds, some with weird timing. Now I get a chime, a vibration, and a little checkmark when I log it. My daughter even gets a notification if I miss a dose. No more guessing. No more guilt. Just peace.
I used to be the guy who took his blood thinner at 8am, then remembered he forgot and took it again at 10am. Twice. Once I ended up in the ER with blood in my urine. Now I have a locked box with my name on it. My meds are color-coded by time of day. I even have a sticky note that says: "IF YOU’RE NOT SURE, DON’T DO IT." I taped it to my fridge. My wife says I’m obsessive. I say I’m alive.
You think this is bad? Try being a diabetic on 12 meds and your pharmacist keeps switching your insulin vials. I’ve had Lantus labeled as Humalog. Twice. I’m not paranoid. I’m just the person who lived through it.
Why are we even talking about this? People who can’t follow five simple rules shouldn’t be allowed to take pills. It’s not rocket science. If you can’t manage your meds, maybe you shouldn’t be living alone. My cousin took her neighbor’s thyroid med and ended up in the ICU. She’s lucky she didn’t die. Some people just aren’t cut out for autonomy.
I used to think meds were like coffee - take it when you remember. Then I got diagnosed with atrial fibrillation and was put on warfarin. Learned the hard way that a 4-hour window isn’t a suggestion. Now I treat my meds like my kid’s school bus schedule - if I miss it, everything falls apart. I’m not a robot. I’m just smarter now.
Interesting how this article assumes everyone has access to pill organizers, smartphones, and pharmacists who answer calls. What about the guy in rural Alabama who drives 90 minutes for his refill and can’t afford a $20 organizer? Or the veteran on VA benefits who gets his meds in a big plastic bag with no labels? The rules are good - but the system’s broken.
ps. dont split pills unless its scored. i once split a 10mg lisinopril because i was broke. ended up with a headache and a bp of 80/50. took me 3 hours to get up. my dog stared at me like i was dead. pharmacy said "next time call us". yeah. next time i’ll just not take it.
The article mentions "brown bag reviews" - but in the UK, GPs rarely offer them. Community pharmacists are overloaded. We need policy change, not just personal responsibility. I’ve seen patients on 17 medications with no coordination between specialists. This isn’t negligence - it’s systemic failure.
While the five rules are sound, I would add a sixth: maintain a relationship with your pharmacist. They are trained medication experts - often more accessible than your doctor. Don’t treat them as order-fillers. Ask them to explain why each drug is prescribed, how it interacts with others, and what to watch for. They’re your silent allies in this process.
I’m 78. I’ve been taking meds since I was 50. I still read every label. I still check the bottle. I still ask questions. I’m not scared of the system. I’m just not stupid. If you’re reading this and you’re younger - start now. Don’t wait until you’re on ten pills and your memory’s gone.