
Every year, millions of people try to quit drinking. Some succeed. Many don’t. And one of the biggest reasons? Medications for alcohol use disorder (AUD) aren’t being used the way they should be - or at all.
If you’re struggling with alcohol dependence, you’ve probably heard that medication can help. But here’s the truth: most people don’t know which ones work, how they work, or why they fail. And worse - doctors often don’t offer them. The result? People try to quit cold turkey, relapse, feel like they’ve failed, and give up. It doesn’t have to be this way.
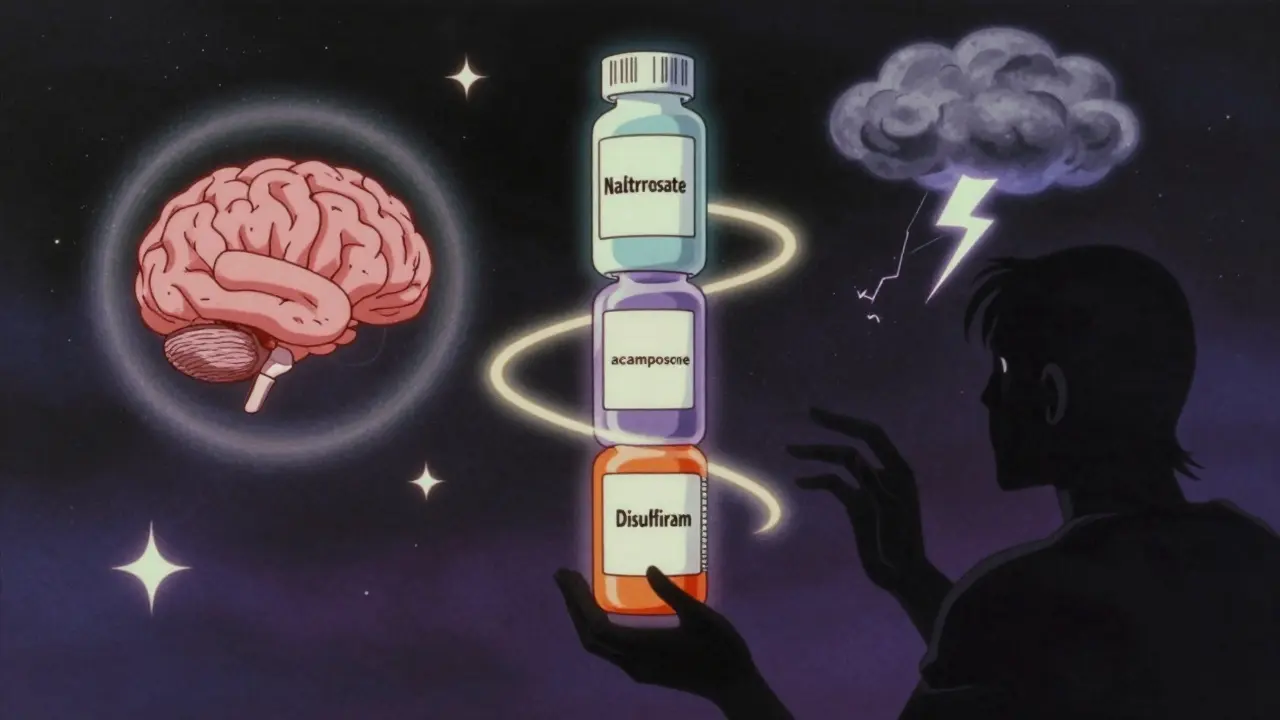
Three FDA-Approved Medications - and How They Actually Work
There are three main medications approved by the FDA to treat alcohol use disorder: acamprosate, naltrexone, and disulfiram. Each works differently. None is a magic pill. But together, they give people real tools to stay sober.
Acamprosate (brand name Campral) doesn’t make you sick if you drink. It doesn’t block cravings. Instead, it helps your brain calm down after you stop drinking. Long-term alcohol use scrambles your brain chemistry - especially the systems that control calm and stress. When you quit, your brain stays wired for chaos. Acamprosate helps restore balance. Studies show it’s most effective for people who’ve already stopped drinking and want to stay stopped. You need at least 3-5 days of abstinence before starting it. Side effects? Mostly mild: diarrhea, upset stomach. About 1 in 10 people quit because of this. But if you can stick with it, it cuts relapse risk by nearly 20%.
Naltrexone (Revia, Vivitrol) works on your brain’s reward system. Alcohol triggers dopamine release - that’s the feeling of pleasure. Naltrexone blocks the opioid receptors that make that happen. So when you drink, it doesn’t feel as good. That reduces cravings and the urge to keep going once you start. Oral naltrexone (50 mg daily) is proven to reduce heavy drinking days by 25-30%. The monthly injection (Vivitrol) is convenient - no daily pills - but studies show it doesn’t help as much as people think. It lowers heavy drinking days, but doesn’t stop you from drinking entirely. Naltrexone can be started even if you’re still drinking. But if you’ve used opioids recently, you need a 7-10 day break first. Liver problems? Watch out. You’ll need monthly blood tests.
Disulfiram (Antabuse) is the oldest - approved in 1951. It’s simple: if you drink alcohol while taking it, you get sick. Really sick. Flushing, vomiting, chest pain, low blood pressure. It’s designed to scare you off drinking. For some people, that fear works. But only if they take it every day. And that’s the problem. Most people stop. Side effects include metallic taste, drowsiness, and liver damage. About 3 in 10 people quit because of it. It’s not for everyone. But for someone highly motivated - say, a professional with a lot to lose - it can be life-changing.
Which Medication Is Right for You?
There’s no one-size-fits-all. The best choice depends on your goals, your body, and your life.
- If your goal is total abstinence and you’ve already stopped drinking, acamprosate is your best bet.
- If you want to cut back on heavy drinking or still drink sometimes but want to stop losing control, naltrexone works better.
- If you’re highly motivated and fear the consequences of drinking, disulfiram might help - but only if you’re ready to take it every single day.
Here’s what experts don’t tell you: gabapentin - a drug usually used for seizures and nerve pain - is becoming a go-to for people with severe withdrawal symptoms. A 2020 study found that among people with a history of intense alcohol withdrawal, gabapentin helped 45% stay abstinent. That’s way higher than placebo. And it’s safer for people with liver disease. If you’ve had seizures or delirium tremens after quitting before, talk to your doctor about gabapentin. It’s not FDA-approved for AUD, but it’s widely used off-label - and it’s cheap.
Why Do So Many People Stop Taking Their Medication?
Even when doctors prescribe these drugs, most people stop within three months. Why?
Cost is a big one. Acamprosate and naltrexone cost $200-$400 a month. Even with insurance, co-pays add up. Disulfiram? $20 a month. But it’s risky. Many people quit because they don’t feel immediate results. They expect to wake up one day and not want to drink. That doesn’t happen. These meds work slowly. You need to take them for weeks before you notice a difference.
Another reason? Shame. People think taking medication means they’re weak. That’s nonsense. You wouldn’t feel guilty about taking insulin for diabetes. Why feel guilty about taking naltrexone for AUD? Addiction is a brain disorder. Medication helps rewire it.
And then there’s the timing. You can’t start acamprosate until you’ve been sober for days. Naltrexone needs a break from opioids. Disulfiram requires a full education on what happens if you drink. If your doctor doesn’t explain this clearly - or if you’re rushed - you’re set up to fail.

The Big Gap: Why Doctors Don’t Prescribe These
Here’s the shocking part: Only 8.6% of Americans with AUD get any medication. That’s not because the drugs don’t work. It’s because most doctors don’t know how to use them.
A survey by SAMHSA found only 28% of primary care doctors feel trained to prescribe AUD meds. Many think addiction treatment belongs in specialty clinics - not their office. But that’s outdated. AUD is a medical condition. Just like high blood pressure or asthma. You don’t need a specialist to manage it - you need a doctor who knows the options.
And it’s not just about prescribing. It’s about follow-up. You need to check in. Adjust doses. Talk about side effects. But most insurance plans don’t cover regular counseling with a doctor for AUD. So patients get a script and vanish.
Combining Medications? Not Always Better
You might think: if one pill helps, two must help more. But the landmark COMBINE study found no extra benefit from combining acamprosate and naltrexone. Taking both didn’t improve outcomes over taking just one.
That doesn’t mean combination therapy never works. One smaller study showed better results with both drugs versus placebo - but not versus naltrexone alone. So if you’re on naltrexone and still drinking heavily, adding acamprosate might not help. But if you’re on acamprosate and still struggling with cravings, naltrexone might be the missing piece.
Bottom line: Don’t stack meds unless your doctor has a clear reason. More isn’t always better.
What’s Next? New Treatments on the Horizon
Science is moving fast. In 2023, a new drug called ALKS 5461 (a mix of buprenorphine and samidorphan) showed a 32% drop in heavy drinking days. It’s not approved yet, but phase 3 trials are promising.
Ketamine infusions - yes, the party drug - are being tested for AUD. In a 2022 trial, three weekly sessions cut relapse rates by 41%. It’s not a cure, but for people who’ve tried everything else, it’s a lifeline.
And then there’s precision medicine. Researchers are now using brain scans to predict who will respond to acamprosate. People with higher frontal white matter integrity? 68% more likely to stay sober on it. Genetic testing is also showing promise. One study found that people with a certain serotonin gene variant had 2.3 times better results with ondansetron - a drug not even approved for AUD yet.
Future treatments? Long-acting naltrexone implants (6-month doses) and smartphone apps that track cravings and remind you to take your pill. One 2023 study showed digital tools cut relapse risk by 33% when paired with medication.
What You Can Do Right Now
If you’re trying to quit drinking and haven’t talked to a doctor about medication, do it now. Don’t wait until you’ve relapsed again.
Ask these questions:
- Do I need to be sober before starting?
- What are the side effects - and how common are they?
- Will I need blood tests?
- Is there a generic version? How much will it cost?
- What happens if I drink while taking it?
And if your doctor says, “Just go to AA” or “Try willpower,” ask why they’re not offering medication. You deserve better.
Medication doesn’t fix everything. You still need therapy, support groups, lifestyle changes. But it gives you the brain chemistry to make those changes stick. For many, it’s the difference between quitting for a week - and staying quit for good.





12 Comments
Finally someone gets it! 🙌 I was on naltrexone for 6 months and it didn’t make me feel like a zombie-just made beer taste like flat soda. Game changer. No more ‘just one’ turning into ‘I don’t remember how I got home.’
My brother took disulfiram for 3 weeks and drank anyway. He said the vomiting was worth it because he got to go to the ER and get free food. I don’t think it works for people who don’t care about consequences.
I think we need to stop treating addiction like it’s a moral failure. It’s a medical condition. If you had diabetes, you wouldn’t be told to ‘just stop eating sugar’-you’d get insulin. Why is alcohol different? The stigma kills more people than the drinking.
Ha. I tried acamprosate. Felt like my brain was wrapped in cotton. Took 3 weeks to notice anything. By then I’d already relapsed. But hey, at least I didn’t die from withdrawal. Progress?
The COMBINE study was flawed. It didn’t account for adherence, nor did it stratify by genetic markers. Modern psychiatry still operates in the Bronze Age. We have fMRI and pharmacogenomics, yet we’re prescribing based on anecdote and habit. Pathetic.
As someone who’s been in recovery for 7 years, I can say with certainty: meds alone don’t work. But meds + therapy + community? That’s the trifecta. I was on gabapentin for 14 months-saved my life. My therapist helped me unpack the trauma behind the drinking. No one thing fixed me. It was the combination.
Why is gabapentin still off-label?! It’s cheaper than coffee, safer than ibuprofen, and works better than half the SSRIs we prescribe for anxiety. Pharma doesn’t profit from generics. That’s why we’re stuck with $400/month pills nobody can afford. This system is broken.
My ex took naltrexone and still got drunk every Friday. Said it made her feel ‘numb but not sober.’ So what’s the point? Just say you’re addicted and move on.
Medication is just a bandage. The real issue is the cultural normalization of alcohol. We glorify drinking in movies, ads, holidays. We call it ‘wine o’clock’ like it’s a wellness ritual. No pill fixes that. Until we stop romanticizing alcohol, we’re just rearranging deck chairs on the Titanic.
Let’s be real-most doctors don’t prescribe because they’re afraid of liability. If you take naltrexone and drink and end up in the ER, who gets sued? The doctor. Not you. So they’d rather say ‘go to AA’ and cover their ass. It’s not ignorance. It’s institutional cowardice.
Respectfully, I must point out that the utilization of pharmacological interventions for alcohol use disorder remains critically underutilized due to systemic healthcare fragmentation and lack of interdisciplinary coordination. Furthermore, the socio-economic determinants of access are often overlooked in clinical discourse.
This is what happens when you let the left turn medicine into a social experiment. We used to have discipline. We used to have willpower. Now we hand out pills like candy and call it ‘compassion.’ You don’t fix a broken soul with chemistry. You fix it with character. And America has lost its character.