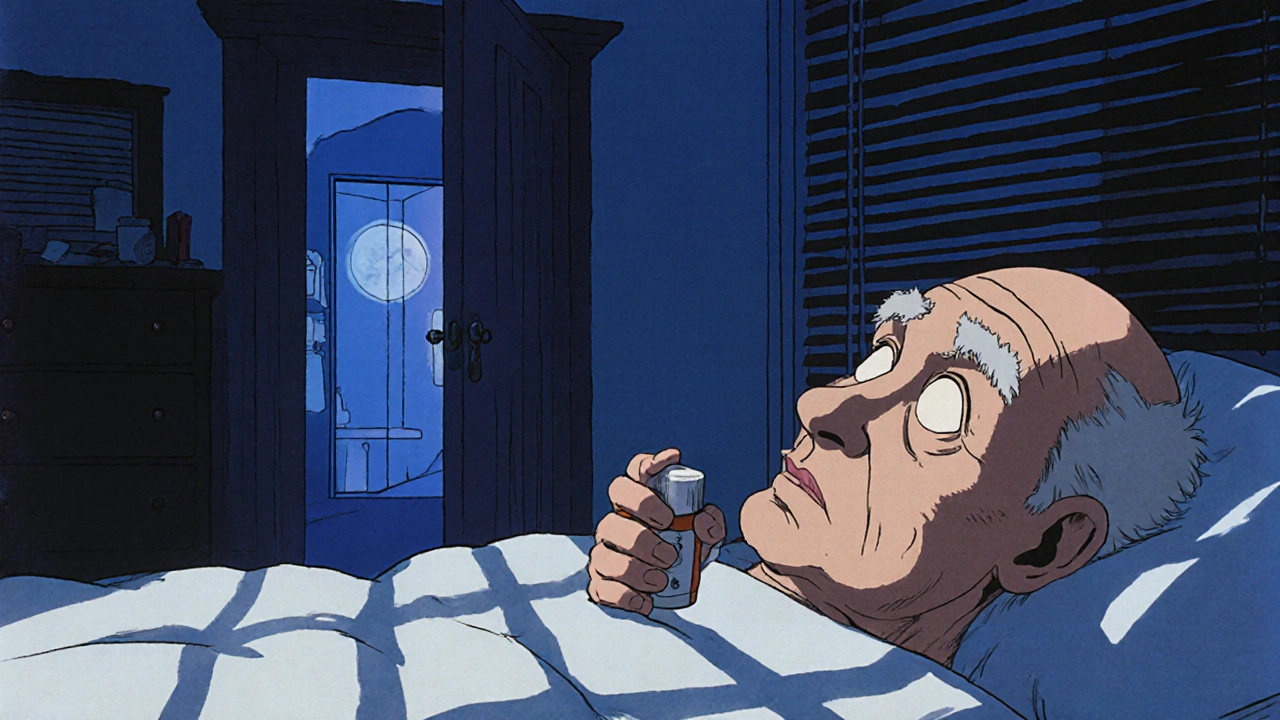
More than 1 in 10 adults over 80 in the U.S. are taking prescription sleep pills every month. But for every person who finds quick relief, another wakes up with no memory of the night before, struggles to get off the medication, or falls in the dark trying to get to the bathroom. Sleep medications might seem like a simple fix for insomnia, but they come with hidden costs that most people don’t realize until it’s too late.
How Sleep Medications Really Work
Sleep meds don’t make you tired-they slow down your brain. Most of them, from Ambien to Lunesta, work by boosting GABA, a calming chemical in your nervous system. This isn’t natural sleep. It’s chemical sedation. Your brain doesn’t go through the normal cycles of deep sleep and REM. You might fall asleep faster, but the quality? Often worse.
There are three main types of prescription sleep drugs. Benzodiazepines like lorazepam and alprazolam were the first, introduced in the 1970s. They’re effective but risky. Z-drugs-zolpidem, eszopiclone, zaleplon-came later as "safer" alternatives. They target the same brain receptors but with slightly less impact on memory and coordination. Then there are off-label options like trazodone and doxepin, originally antidepressants, now used because they’re cheap and easy to prescribe.
Over-the-counter sleep aids? They’re antihistamines. Benadryl and Unisom. These aren’t sleep meds-they’re allergy pills that make you drowsy. They block acetylcholine, a key brain chemical. Long-term use? That’s linked to a 54% higher risk of dementia, according to a major JAMA study.
The Hidden Dangers You’re Not Being Told
The FDA issued a black box warning for zolpidem in 2019. That’s the strongest warning they give. Why? Because people were sleep-driving, sleep-eating, even sleep-calling 911-without remembering any of it. One in 200 users of Z-drugs has experienced one of these complex sleep behaviors. That’s not rare. That’s common enough that doctors should screen for it.
Next-day drowsiness hits 31% of users. That’s not just feeling a little tired. That’s impaired reaction time, poor focus, and memory lapses. Studies show the mental fog after taking a sleep pill is like having a blood alcohol level of 0.05%-right at the legal limit for driving in many places. And yet, people take these pills and go to work, drive their kids to school, or operate machinery the next morning.
For older adults, the risks are even worse. The American Geriatrics Society says these drugs should be avoided entirely after age 65. Why? Because they increase fall risk by 50-60%. A single fall can mean a broken hip, months in rehab, and loss of independence. In 2023, over 18,000 emergency room visits in the U.S. were linked to sleep medication side effects in seniors.
Dependence Is Faster Than You Think
Most people think they can just stop when they’re ready. But dependence builds quietly. After just 2-3 weeks of nightly use, your brain starts to rely on the drug to shut down. When you skip a dose, your nervous system goes into overdrive. Rebound insomnia hits hard-worse than before you started.
Studies show up to 33% of people on benzodiazepines become dependent after six weeks. Z-drugs are lower risk, but still 5-10%. That’s 1 in 10 to 1 in 20 people who can’t quit without help. Reddit threads from insomnia communities are full of stories like this: “Took Ambien for 6 months. Tried to quit. Couldn’t sleep for 3 nights. Ended up right back on it.”
Doctors rarely warn you about this. They write the prescription, tell you to take it at night, and move on. But the withdrawal can be brutal-anxiety, tremors, nightmares, even seizures in extreme cases. Tapering off needs to be slow: 25% reduction every two weeks, under medical supervision. And even then, 40% of people need extra support to get off.
What Actually Works Better-And Why
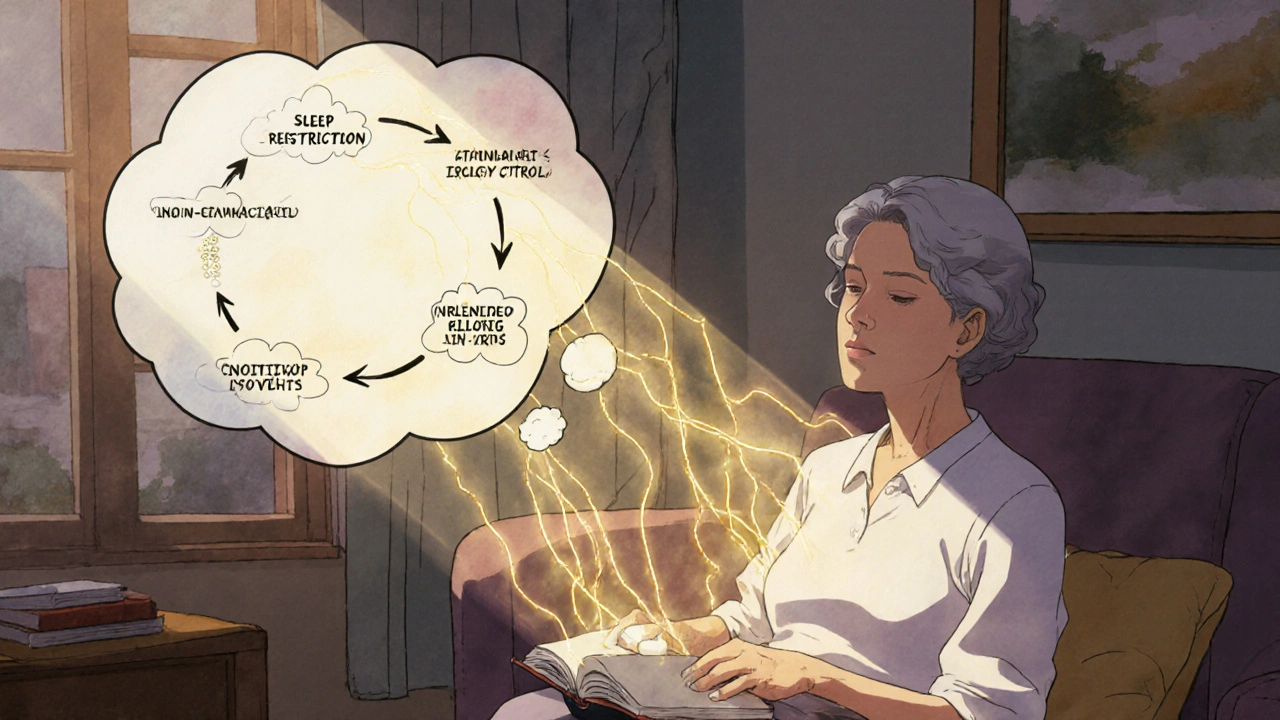
There’s a treatment that works better than any pill. It’s called CBT-I-Cognitive Behavioral Therapy for Insomnia. It’s not magic. It’s not a gadget. It’s a structured program that retrains your brain and body to sleep naturally.
CBT-I doesn’t use drugs. It teaches you to fix the thoughts and habits keeping you awake. You learn sleep restriction (only being in bed when sleepy), stimulus control (using the bed only for sleep and sex), and how to quiet racing thoughts. It’s not quick. It takes 4-8 weeks. But the results? 70-80% of people see lasting improvement. And unlike pills, the benefits stick around for years.
A 2021 JAMA study found that people using a digital CBT-I app called Somryst had a 60% remission rate after 12 weeks. That’s better than most sleep meds. And no hangover. No dependence. No risk of falling.
And yet, only 1 in 5 doctors even mention CBT-I as a first option. Why? Because it takes time to teach. Pills are fast. Insurance often won’t cover CBT-I unless you’ve tried medication first. That’s backwards.
Alternatives That Actually Help
If you’re looking for something between a pill and a therapy program, here’s what science supports:
- Melatonin: Not a sleep drug. It’s a hormone that signals nighttime. Works best for jet lag or shift work. Dose? 0.5mg to 3mg, taken 2 hours before bed. Higher doses don’t help more-they just make you groggy.
- Valerian root: Some studies show mild improvement in sleep quality. Not strong, but low risk. Take 400-900mg an hour before bed.
- Magnesium glycinate: Helps calm the nervous system. 200-400mg at night. Especially helpful if you have muscle cramps or anxiety.
- Good sleep hygiene: No screens 1 hour before bed. Cool, dark room. Consistent wake-up time-even on weekends. This sounds basic, but 80% of people skip it.
Don’t waste money on “natural sleep gummies” loaded with sugar and unproven herbs. Stick to what’s been tested. And remember-none of these work like a pill. They’re supports, not shortcuts.
When Medication Might Still Make Sense
Let’s be real. Sometimes, you need a pill. If you’re dealing with acute insomnia after a divorce, a death, or a major life change, a short course of medication can give you breathing room. But it should be exactly that-short. Two weeks max. And paired with a plan to start CBT-I before you stop.
For people with severe depression or chronic pain, sleep meds can be part of a broader treatment plan. But even then, experts agree: medication should never be the only tool. Always combine it with behavioral support.
The new frontier? Orexin blockers like Quviviq. These drugs target a different brain pathway-less sedation, less next-day fog. Early data shows they’re safer than Z-drugs. But they’re expensive, and we still don’t know the long-term effects.
What to Do Right Now
If you’re on sleep medication:
- Don’t quit cold turkey. Talk to your doctor about tapering.
- Ask for a referral to a sleep specialist or CBT-I provider. Many are covered by insurance now.
- Track your sleep for a week-no pills. Use a simple notebook or phone app. You might be surprised how much better you sleep without them.
- Eliminate alcohol at night. It makes sleep meds 300% more dangerous and ruins sleep quality.
- Set a bedtime alarm. Not to wake up-to go to bed. Consistency is the most powerful sleep tool you have.
If you’re thinking about starting:
- Ask your doctor: "Is CBT-I an option?" If they say no, ask why.
- Request the lowest possible dose for the shortest time.
- Get a written plan for how to stop, not just how to take it.
Sleep isn’t a problem to be fixed with a pill. It’s a natural process that got disrupted. The best solutions don’t come in a bottle-they come from changing habits, thoughts, and routines. The science is clear. The safest, most effective way to sleep well? It’s not a prescription. It’s a lifestyle.
Can sleep medications cause dementia?
Yes-specifically over-the-counter antihistamines like diphenhydramine (Benadryl) and doxylamine (Unisom). A major study in JAMA Internal Medicine found a 54% higher risk of dementia after long-term use. Prescription sleep drugs like benzodiazepines and Z-drugs are also linked to cognitive decline in older adults, especially when used for more than 3 months. The mechanism involves blocking acetylcholine, a key brain chemical for memory and learning.
How long does it take to get addicted to sleep pills?
Dependence can develop in as little as 2 to 3 weeks of nightly use. Benzodiazepines carry the highest risk-up to 33% of users become dependent after 4 to 6 weeks. Z-drugs like Ambien and Lunesta are lower risk, but still about 5-10%. The body adapts quickly. When you stop, your brain struggles to shut down without the drug, leading to rebound insomnia and anxiety. This often traps people into continuing use.
Is melatonin a safe alternative to sleep medication?
Melatonin is generally safe for short-term use and works best for circadian rhythm issues like jet lag or shift work. It doesn’t cause dependence or next-day grogginess. But it’s not a strong sleep inducer for chronic insomnia. Doses higher than 3mg don’t help more-they just increase side effects. Look for 0.5mg to 1mg, taken 2 hours before bed. Avoid gummies with added sugar or unregulated ingredients.
What is CBT-I, and why is it better than pills?
CBT-I stands for Cognitive Behavioral Therapy for Insomnia. It’s a structured program that changes the thoughts and behaviors keeping you awake. Unlike pills, it doesn’t sedate your brain-it rewires your sleep patterns. Studies show 70-80% of people improve long-term, with results lasting years. It has no side effects, no dependence risk, and works better than medication over time. The downside? It takes 4 to 8 weeks to see results, and not all doctors offer it.
Can I drive the morning after taking a sleep pill?
No. Even if you feel fine, your reaction time, coordination, and alertness are impaired. The FDA issued a safety warning in 2019 after multiple reports of people driving while still under the influence of zolpidem. Studies show the mental impairment is equivalent to a blood alcohol level of 0.05% to 0.08%-the legal limit in many places. Always allow 7 to 8 hours of sleep after taking a sleep pill, and never drive if you feel drowsy.
Why are sleep medications still prescribed so often if they’re risky?
Because they’re fast, easy, and profitable. A doctor can write a prescription in 30 seconds. CBT-I requires referrals, training, and time-things most clinics don’t have. Insurance often blocks CBT-I unless you’ve tried medication first. Pharmaceutical companies spend billions marketing sleep pills. Meanwhile, behavioral therapies are underfunded and under-promoted. The system is built to treat symptoms, not fix causes.
What’s the safest way to stop taking sleep medication?
Never quit cold turkey. Work with your doctor to create a tapering plan-usually reducing the dose by 25% every two weeks. Use a sleep diary to track progress. Add CBT-I techniques during the taper to manage rebound insomnia. Some people need support from a sleep specialist or therapist. About 40% of users need extra help to quit successfully. If you experience severe anxiety, tremors, or hallucinations during withdrawal, seek medical help immediately.
For anyone who’s spent nights staring at the ceiling, the truth is this: you don’t need a pill to sleep. You need the right tools, the right habits, and the right support. The science is here. The options exist. The only thing missing is the willingness to try something that doesn’t come in a bottle.


11 Comments
This is the kind of post that should be mandatory reading for every doctor and every person over 50. 🙏 I’ve seen so many older relatives get hooked on Ambien and never look back. CBT-I changed my life - took 6 weeks, no pills, now I sleep like a baby. 🌙💤
The data presented here is unequivocal. Prescription hypnotics confer significant cognitive and physical risks disproportionate to their transient benefits. The persistence of their prescription reflects systemic failures in medical education and pharmaceutical influence.
lol so now we’re supposed to believe some therapist with a clipboard can fix sleep better than a pill? 🤡 my grandpa took zolpidem for 12 years and still drove his truck to the feed store every morning. wake up sheeple
Let’s be honest - this isn’t about sleep. It’s about control. The pharmaceutical-industrial complex has spent decades convincing us that natural rhythms are broken and must be fixed with chemicals. Meanwhile, the same entities fund the FDA, the AMA, and even ‘independent’ sleep studies. CBT-I? A distraction. The real solution? Stop eating processed carbs after 6pm and turn off the blue light. But that wouldn’t sell pills, would it?
CBT-I sounds nice but who has time? I work 12-hour shifts, raise 2 kids, and my wife snores like a chainsaw. 🤷♂️ I take 5mg melatonin and call it a day. If it works, why overthink it? Also, the FDA is just another branch of Big Pharma anyway.
We’ve been sold a lie. Sleep isn’t a problem. It’s a metaphor. You don’t need to fix your sleep - you need to stop running from your life. The pills? They’re just a Band-Aid on a bullet wound. 🌑✨ CBT-I? That’s the therapy for the soul. But nah, let’s just keep popping pills and pretending we’re productive.
The science here is solid. But I think the deeper issue is cultural. We live in a world that rewards constant output. Sleep is seen as wasted time. So we reach for chemical shortcuts instead of relearning how to rest. It’s not about pills. It’s about a society that has forgotten how to be still.
The neuropharmacological mechanism of GABAergic modulation in Z-drugs is indeed distinct from natural sleep architecture, which involves dynamic oscillations between NREM and REM phases. The downregulation of endogenous melatonin receptors due to chronic exogenous administration is a documented phenomenon. That said, CBT-I demonstrates a robust effect size (Cohen’s d = 0.82) in RCTs, with durable outcomes at 12-month follow-up. Recommend integrating stimulus control protocols with sleep restriction for optimal neuroplastic adaptation.
I was skeptical too - until I tried CBT-I. My therapist had me write down every thought that kept me awake. Turns out I was stressing about work emails I hadn’t even sent. 🤦♂️ It took 5 weeks, but now I sleep without anything. No pills. No guilt. Just peace. You got this.
Melatonin is just a hormone. Hormones are for cows. 🐄 If you’re not willing to sit with your anxiety and rewire your brain, then yes - take the pill. But don’t pretend you’re ‘doing something healthy.’ You’re just outsourcing your discomfort to a chemist in New Jersey.
I’ve been on these pills for 3 years. I thought I was fine. Then I fell in the bathroom at 3 a.m. and broke my wrist. I didn’t even remember getting up. I’m quitting. I’m doing CBT-I. I’m turning off my phone at 9 p.m. I’m done pretending I’m a superhero who doesn’t need sleep. I need rest. And I’m taking it back. 💪🌙