
Living with IBS-Mixed means your gut feels like a switch-some days you’re stuck, others you’re running to the bathroom. There’s no warning. No pattern you can count on. One morning you’re struggling to pass a hard stool, and by lunch, you’re in the bathroom again with watery diarrhea. It’s exhausting. And confusing. You try a laxative, and it makes the diarrhea worse. You take an antidiarrheal, and now you’re bloated and backed up. You’re not alone. About 1 in 5 people with IBS have this mixed pattern, and most of them spend years trying to figure out what works.
What Exactly Is IBS-Mixed?
IBS-Mixed, or IBS-M, isn’t just "bad digestion." It’s a specific diagnosis defined by the Rome IV criteria: recurrent abdominal pain at least once a week for three months, linked to changes in bowel habits-and you must have both constipation and diarrhea in at least 25% of your bowel movements. That means you’re seeing Type 1 or 2 stools (hard lumps or sausage-shaped but lumpy) and Type 6 or 7 (watery or entirely liquid) on the Bristol Stool Scale. This isn’t occasional upset stomach. It’s a pattern that repeats over months.
Unlike Crohn’s or ulcerative colitis, IBS-M doesn’t show inflammation on a colonoscopy. There’s no tumor, no bleeding, no structural damage. The problem lies deeper-in how your gut nerves react, how fast food moves through your intestines, and how your gut bacteria are balanced. Stress, food, and even sleep can trigger it. And because your symptoms flip-flop, treatment gets tricky. What helps one week can wreck the next.
Why Standard IBS Treatments Often Fail
Doctors used to treat IBS like it was one condition. Give a laxative for constipation. Give Imodium for diarrhea. But with IBS-M, that approach backfires. A 2018 study showed that linaclotide, a drug approved for IBS-C, only helped 22% of IBS-M patients. Eluxadoline, designed for IBS-D, worked for just 19% of those with mixed symptoms. Why? Because these drugs target one side of the problem-and IBS-M needs both sides addressed.
Over-the-counter meds make things worse for many. A survey of 1,200 IBS-M patients found that 38% said loperamide (Imodium) made their constipation worse. Another 32% said laxatives triggered sudden diarrhea. You’re not doing anything wrong. You’re just using tools built for a different kind of IBS.
The real issue? Most people wait 6 to 7 years to get a correct diagnosis. They see three or four doctors. They get tested for celiac disease, colon cancer, infections. All come back normal. Then they’re told, "It’s just stress." But it’s not. It’s real. And it’s manageable-with the right plan.
The Low FODMAP Diet: Your Best Shot at Control
The most proven dietary tool for IBS-M is the low FODMAP diet. FODMAPs are short-chain carbs that ferment in your gut and pull water in, causing bloating, gas, and erratic bowel movements. High-FODMAP foods include onions, garlic, wheat, dairy, apples, honey, and artificial sweeteners.
A 2021 study in Gastroenterology tracked 215 IBS patients. Those on the low FODMAP diet saw symptom improvement in 50-60% of IBS-M cases. That’s lower than the 70-75% seen in IBS-D, but still the best result you’ll get from diet alone. Reddit users report similar results: 62% say it helped them most. One user, u/SarahIBS2022, cut her symptom days from 25 to 8 per month after three months of strict low FODMAP eating and daily peppermint oil capsules.
But here’s the catch: you can’t stay on the strict elimination phase forever. It’s too restrictive. You need to rebuild your diet. That means a 2-6 week elimination, followed by 8-12 weeks of carefully reintroducing one FODMAP group at a time. Which foods trigger you? Is it apples? Or wheat? Or both? A registered dietitian who specializes in IBS can guide you through this. Monash University’s app is a trusted tool for checking FODMAP levels in foods.
And don’t assume you have to cut everything forever. Many people find they can tolerate small amounts of certain triggers. The goal isn’t perfection. It’s control.
Medication: The Right Tools for the Right Day
Because your symptoms alternate, you need two medications on hand-not one.
- For constipation: Polyethylene glycol (Miralax, 17g daily) is gentle, doesn’t cause cramping, and doesn’t lead to rebound diarrhea. Avoid stimulant laxatives like senna-they can trigger sudden bowel movements.
- For diarrhea: Loperamide (Imodium, 2-4mg as needed) is effective, but use it sparingly. Too much can cause constipation or bloating. Don’t take it daily.
Antispasmodics like dicyclomine (10-20mg as needed) help with cramping and pain across all IBS types. About half of IBS-M patients find relief with this. They don’t fix constipation or diarrhea, but they take the edge off the pain that makes everything worse.
Antidepressants are surprisingly effective. Tricyclics (like amitriptyline, 10-50mg at night) work better than SSRIs for IBS-M. They don’t treat depression-they help calm overactive gut nerves. Studies show 55-60% of IBS-M patients see reduced pain and better bowel control. It’s not a mood drug. It’s a nerve-calming tool.
Enteric-coated peppermint oil (like IBgard) is another option. It relaxes gut muscles and reduces bloating. Reviews show 68% of IBS-M users report less pain and 57% less bloating. Some get heartburn, but it’s rare. Take it 30 minutes before meals.
Stress Isn’t the Cause-But It’s the Spark
Stress doesn’t cause IBS-M. But it lights the fuse. A 2019 study found 68% of IBS-M patients say stress makes their symptoms worse. That’s why therapy isn’t optional-it’s essential.
Cognitive Behavioral Therapy (CBT) is the most researched psychological treatment. A 2021 guideline from the American Gastroenterological Association found CBT reduced symptom severity by 40-50% in IBS-M patients. That’s better than most medications. You’re not "going crazy." You’re training your brain to respond differently to gut signals.
Apps like Cara Care and Nerva offer guided CBT programs designed for IBS. They teach you how to notice stress triggers, reframe anxious thoughts, and use breathing techniques to calm your gut. One study showed patients using these apps improved 35% more than those using paper diaries.
Even simple mindfulness practices-10 minutes of deep breathing before bed-can help. Your gut has its own nervous system. When your mind is calm, your gut follows.
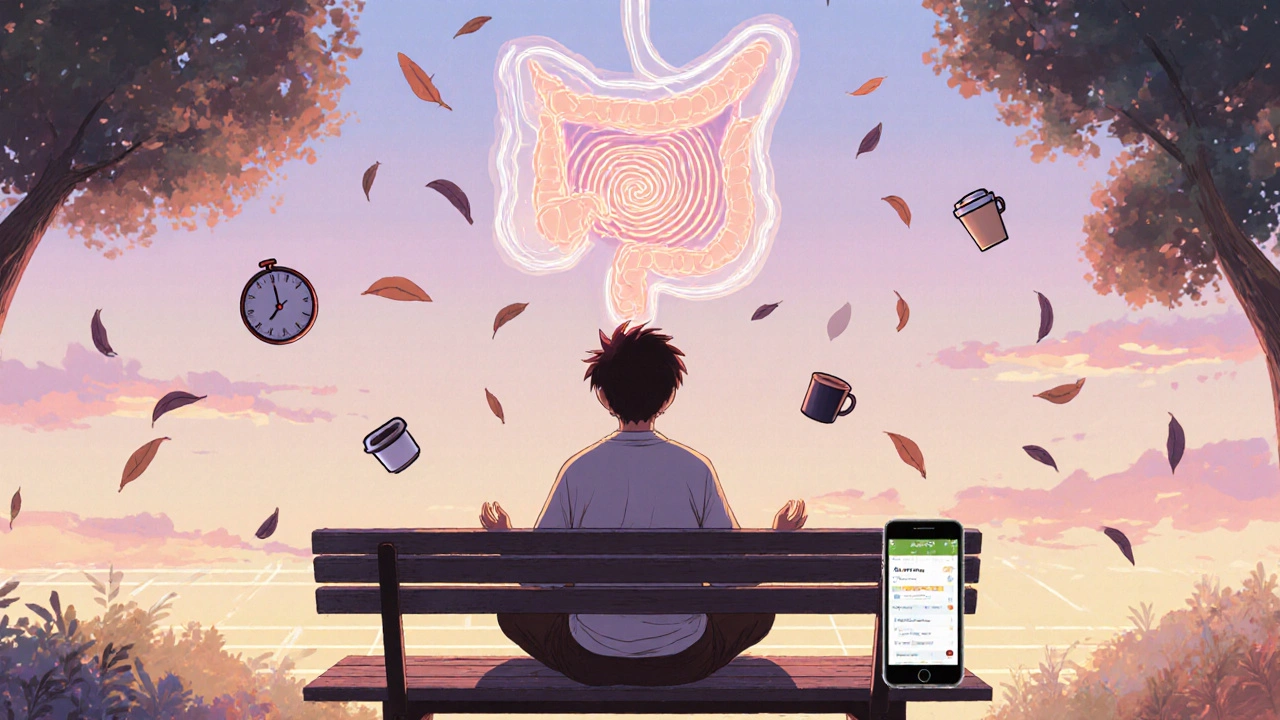
Tracking Your Symptoms: The Key to Personalized Control
You can’t manage what you don’t measure. A symptom diary isn’t optional. It’s your roadmap.
Track every day for at least four weeks:
- Bowel movement type (use the Bristol Stool Scale)
- Pain level (0-10)
- Food and drinks consumed
- Stress level (low, medium, high)
- Medications taken
Look for patterns. Do your diarrhea days follow coffee? Do constipation flares happen after dairy? Do pain spikes happen after stressful meetings? You’ll start to see your triggers. That’s power.
Apps like Cara Care, GI Buddy, or even a simple Google Sheet make this easier than paper. One 2022 study found digital tracking led to 35% better symptom improvement than paper logs. You don’t need to be perfect. Just consistent.
What Doesn’t Work (And Why)
Don’t waste time on these:
- Gluten-free without celiac: If you don’t have celiac disease, cutting gluten won’t help unless you’re also cutting wheat-which is high in FODMAPs. The benefit comes from removing fructans, not gluten.
- Probiotics without targeting: Not all probiotics help. The strain matters. Bifidobacterium infantis 35624 (Align) has shown benefit in IBS-M. Others? No proof.
- Extreme diets (keto, paleo): They’re too restrictive and often high in fat, which worsens IBS symptoms.
- Detoxes and cleanses: They disrupt your gut even more. Your body cleans itself.
Also, avoid taking multiple meds at once. That’s how you end up with constipation from Imodium and diarrhea from Miralax. Pick one for each symptom and use it only when needed.
What’s New in IBS-M Treatment
Science is moving fast. In 2023, the FDA approved a new drug called ibodutant, a neurokinin-2 receptor blocker. In phase 3 trials, it improved global symptoms in 45% of IBS-M patients-compared to 28% with placebo. It’s not on the market yet, but it’s promising.
Microbiome testing is also advancing. Companies like Viome use AI to analyze your gut bacteria and suggest personalized diets. In a 2023 pilot, users saw 58% symptom improvement. It’s expensive, but for those who’ve tried everything else, it’s a game-changer.
The Rome V criteria, coming in 2024, will raise the bar for diagnosis: instead of 25% alternating stools, you’ll need 30%. That means fewer false positives and more accurate treatment.
How Long Until You Feel Better?
There’s no quick fix. But most people see improvement within 3-6 months of sticking to a plan. One study found 70% of IBS-M patients reported significant relief after mastering symptom tracking and trigger identification.
It’s not about being symptom-free. It’s about reducing flare-ups, knowing what to do when they happen, and regaining control over your life. You won’t need to cancel plans. You won’t dread meals. You’ll know what to eat, what to avoid, and what to take when things go sideways.
IBS-M is complicated. But you’re not broken. You just need the right system-and you already have the first step: you’re looking for answers. That’s more than most people do.
Can IBS-Mixed turn into Crohn’s or ulcerative colitis?
No. IBS-M is a functional disorder, not an inflammatory one. It doesn’t cause damage to the intestinal lining or increase cancer risk. If you’re worried about inflammation, your doctor should check for celiac disease, Crohn’s, or infections with blood tests and stool markers before diagnosing IBS-M.
Why do my symptoms change so quickly-from constipation to diarrhea?
Your gut motility is unstable. Stress, food triggers, or even changes in sleep can speed up or slow down how fast your intestines move. In IBS-M, the nerves controlling these movements are oversensitive. One day, they’re sluggish (constipation); the next, they’re overactive (diarrhea). It’s not random-it’s your nervous system reacting unpredictably.
Should I take fiber supplements?
Yes-but only soluble fiber. Psyllium husk (Metamucil) is safe and helps both constipation and diarrhea by absorbing water and forming a gel. It smooths out bowel movements. Avoid insoluble fiber like wheat bran-it can irritate your gut and worsen bloating.
Is IBS-Mixed more expensive to treat than other types?
Yes. IBS-M patients spend about 18% more on healthcare than those with IBS-C or IBS-D. Why? Because they need more doctor visits, more tests, and often two or more medications. They also miss more work and use more over-the-counter remedies.
Can I ever eat normally again?
Yes. The low FODMAP diet is a temporary tool. After identifying your triggers, you’ll slowly add back foods you tolerate. Many people end up eating 80-90% of their old diet-with just a few triggers avoided. It’s not forever. It’s a learning phase.
Are there any natural remedies that actually work?
Yes. Peppermint oil (enteric-coated), probiotics like Align, and magnesium citrate (for constipation) have solid evidence. Ginger tea helps with nausea and cramping. Avoid herbal laxatives like senna or cascara-they’re too harsh. Stick to what’s been studied.
If you’ve tried everything and still feel stuck, don’t give up. IBS-M is hard, but it’s not hopeless. The right combination of diet, medication, and mindset can get you back to living-not just surviving.




8 Comments
low fodmap worked for me but only if i skipped coffee and wine
other than that i was still screwed
Thank you for sharing this so clearly. Many people feel alone with IBS-M, but your post reminds us that there are real, research-backed ways to manage it. Small steps like tracking symptoms and using peppermint oil can make a big difference over time. You're not broken-you're learning.
Let me be perfectly clear: the entire low-FODMAP paradigm is a placebo-driven illusion perpetuated by pharmaceutical adjuncts and Monash University’s marketing arm. The real culprit? Glyphosate residue in gluten-free oats, which disrupts the gut-brain axis via epigenetic methylation. No peer-reviewed study has isolated FODMAPs as a primary variable-only confounding dietary variables. And don’t get me started on the FDA’s suppression of ibodutant’s phase 3 data. The system is rigged.
Okay so I’ve been dealing with this for 12 years and I swear to god it’s not just my gut-it’s the EMFs from my smart meter, the fluoride in the water, and the fact that my ex’s ghost is still haunting my apartment because I never returned his favorite hoodie and now my colon is paying the price
every time I eat a banana I feel like I’m being judged by the spirit of a 1998 gastroenterologist who said ‘it’s all in your head’ and then died of a heart attack right after writing that note
and I tried the low FODMAP diet and it worked for two weeks until I accidentally ate a mushroom and then I cried for three days straight and my cat stopped talking to me
also I think the government is using IBS-M to test population-wide stress responses via WiFi and I’m not crazy I’ve seen the documents
it’s not just IBS it’s a conspiracy and I’m the only one who sees it
i tried miralax and it helped with the constipation but i forgot to drink enough water and got really bloated
also peppermint oil gave me heartburn 😅
but tracking with gil buddy actually helped me spot the coffee trigger
still figuring it out though
This is the most helpful post I’ve read in years. Thank you.
Given the neurovisceral dysregulation inherent in IBS-M, the autonomic nervous system's bidirectional signaling via the enteric nervous system necessitates a multimodal therapeutic approach. The vagal tone modulation achieved through CBT and enteric-coated peppermint oil aligns with current neurogastroenterological frameworks. Furthermore, the exclusion of fermentable oligo-, di-, monosaccharides, and polyols (FODMAPs) remains the only evidence-based dietary intervention with reproducible clinical outcomes in randomized controlled trials. I would strongly recommend adherence to the Monash protocol with serial reintroduction under dietetic supervision.
While the author presents a coherent synthesis of current literature, it is regrettable that the post fails to acknowledge the limitations of the Rome IV criteria in capturing phenotypic heterogeneity. The forthcoming Rome V criteria, which increase the threshold for alternating bowel habits from 25% to 30%, are not merely a refinement-they represent a necessary recalibration of diagnostic precision. Moreover, the uncritical endorsement of Miralax as a benign agent overlooks its potential to induce electrolyte imbalance with prolonged use. A more rigorous discussion of pharmacokinetic profiles is warranted.