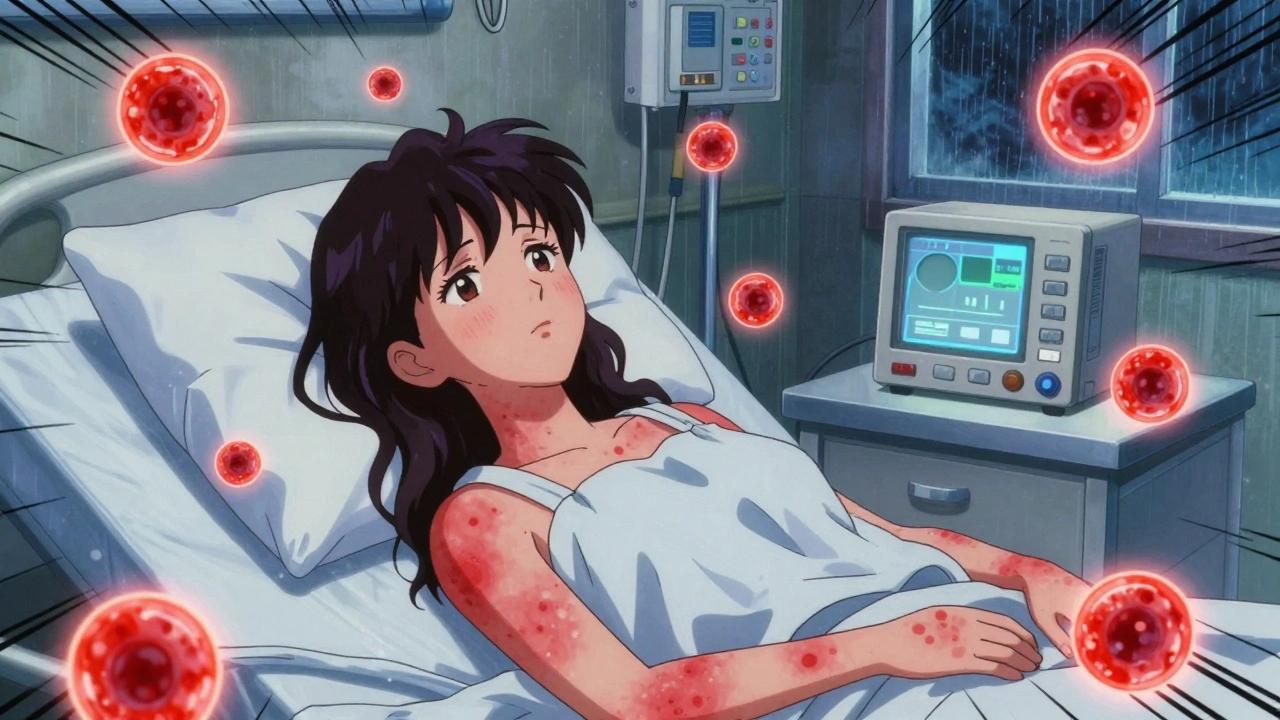
Most people think of side effects from medications as a rash, upset stomach, or drowsiness. But some drug reactions go far beyond that. One of the most dangerous is DRESS syndrome - Drug Reaction with Eosinophilia and Systemic Symptoms. It doesn’t just cause a skin rash. It can shut down your liver, damage your kidneys, and even kill you if it’s not caught early. And here’s the scary part: it often shows up weeks after you start a new drug. By the time you feel really sick, the damage is already done.
What DRESS Syndrome Actually Looks Like
DRESS isn’t a simple allergy. It’s a full-body immune system meltdown triggered by certain drugs. The classic signs show up in stages. First, you might feel like you’re coming down with the flu: fever over 38°C, sore throat, swollen glands, and extreme tiredness. Then, after a few days, a rash appears - usually red, flat, and spread out like measles. It’s not itchy at first, but it can get worse. About 80% of cases start with this kind of rash.
But the real red flags aren’t on your skin. They’re in your blood. Nearly every patient with DRESS has high levels of eosinophils - a type of white blood cell that normally fights parasites. In DRESS, these cells go wild and start attacking your organs. At the same time, you’ll often see abnormal lymphocytes in your blood, which means your immune system is confused and overreacting.
What makes DRESS so dangerous is how many organs it can hit. The liver is the most common target. In 70 to 90% of cases, liver enzymes like ALT spike above 1,000 U/L - that’s more than 20 times the normal level. Your kidneys can fail. Your lungs can fill with fluid. Your heart can get inflamed. Even your thyroid can go haywire. Some people develop Graves’ disease months after their DRESS clears up.
Which Drugs Cause DRESS?
Not every drug causes this. But a few are well-known triggers. Allopurinol, the medicine used to treat gout, is the biggest culprit. It causes 40 to 50% of all DRESS cases. That’s especially true if you have kidney problems. If your eGFR is below 60, your risk jumps to 1 in 200.
Antiepileptic drugs like carbamazepine, phenytoin, and lamotrigine are next on the list. These are often taken for years without issue - until suddenly, they aren’t. Sulfonamide antibiotics like sulfamethoxazole (in Bactrim) are also common triggers. Even some antivirals and blood pressure meds have been linked.
The timing is weird. Most drug allergies happen within hours or days. DRESS takes weeks. It usually shows up between 2 and 8 weeks after you start the drug. Some cases appear as late as 16 weeks. That’s why so many doctors miss it. They think, “It’s been weeks - it can’t be the medicine.” But that delay is exactly what makes DRESS so deadly.
DRESS vs. Other Serious Skin Reactions
People often confuse DRESS with Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). All three are rare, dangerous, and drug-triggered. But they’re not the same.
- SJS/TEN: Skin blisters and peels off in large sheets. Mucous membranes (mouth, eyes, genitals) are almost always involved. Onset is fast - within 1 to 4 weeks. Death rate is 30-40% for TEN.
- DRESS: Skin rash is more like a widespread measles outbreak. Peeling is rare. Mucosal damage happens in only 30-50% of cases. But internal organs are heavily involved. The death rate is around 10% - lower than TEN, but still serious.
The immune systems behind them are different too. SJS/TEN are driven by killer T-cells that directly destroy skin cells. DRESS is fueled by eosinophils and CD4+ T-cells that trigger inflammation throughout the body. That’s why steroids work better for DRESS than for SJS/TEN.
Why It’s So Often Missed
A 2020 study found that only 35% of internal medicine residents could correctly identify a DRESS case. Why? Because the symptoms look like so many other things - viral infections, mononucleosis, even Lyme disease. The rash can mimic chickenpox. The fever and swollen glands look like a bad flu. And if your liver enzymes are high, doctors might blame alcohol, hepatitis, or fatty liver.
Patients report seeing three or more doctors before getting the right diagnosis. One woman in her 50s took allopurinol for gout. After three weeks, she developed a rash, fever, and jaundice. Her first doctor said it was a viral infection. The second thought it was gallstones. The third finally ordered a full blood panel and found her eosinophils were over 3,000. She spent 45 days in the hospital. Her liver enzymes peaked at 2,840 U/L. She survived - but barely.
And here’s another twist: in 60 to 70% of DRESS cases, the body reactivates a dormant virus - HHV-6, the same one that causes roseola in babies. This virus flare-up might actually make the reaction worse and last longer. It’s like your immune system is fighting both the drug and the virus at the same time.
What Happens After Diagnosis
If DRESS is suspected, the first and most critical step is stopping the drug - immediately. Delaying by even 24 hours can raise your risk of death from 5% to 15%. No exceptions. No waiting to see if it gets better.
You’ll need to be hospitalized. Most patients stay 14 to 21 days. Doctors will monitor your liver, kidneys, and blood counts daily. Infections are common because your skin is broken and your immune system is exhausted. Bacteria like MRSA and fungi like Candida can sneak in.
Most people get corticosteroids - usually prednisone or methylprednisolone. The dose is high at first (0.5 to 1 mg per kg of body weight) and then slowly tapered over 4 to 8 weeks. Stopping too soon can cause a rebound reaction. Some patients need IV steroids if their liver or lungs are failing.
There’s new hope on the horizon. A 2022 study showed that adding anakinra (a drug used for rheumatoid arthritis) to steroids cut hospital stays from 18.5 days to just 11.2 days. Clinical trials are now testing tocilizumab for patients who don’t respond to steroids. These aren’t standard yet, but they’re promising.

Long-Term Risks and What Comes Next
DRESS doesn’t always end when the rash fades. About 20 to 30% of survivors have lasting organ damage. Kidney problems are the most common - many need ongoing nephrology care. Some develop autoimmune diseases like thyroiditis, lupus, or type 1 diabetes months or even years later.
One patient on Reddit described developing Graves’ disease five weeks after her DRESS cleared up. Her thyroid went into overdrive. She needed radioactive iodine treatment. That’s not rare. Studies show 5 to 10% of DRESS survivors develop autoimmune conditions.
Genetics play a big role too. If you’re of Asian descent and carry the HLA-B*58:01 gene, your risk of allopurinol-induced DRESS is 55 times higher. That’s why Taiwan now requires genetic testing before prescribing allopurinol. Since 2020, the FDA recommends the same for people with kidney disease. The result? A 75% drop in cases in places that use screening.
Doctors are now shifting away from allopurinol for patients with poor kidney function. Febuxostat is becoming the first-choice drug for gout in these cases. It’s not perfect, but it doesn’t trigger DRESS the same way.
What You Should Do
If you’re taking any of these drugs - allopurinol, carbamazepine, lamotrigine, phenytoin, or sulfonamides - and you develop a fever and rash more than a week after starting the medicine, don’t wait. Go to the ER. Tell them you’re worried about DRESS. Bring a list of all your medications.
If you’ve had DRESS before, never take the same drug again. And avoid similar ones. For example, if carbamazepine caused it, don’t take oxcarbazepine or phenytoin. Cross-reactivity is common.
Keep a medical alert card or phone note listing your trigger drugs. Share this with every new doctor. Even if you feel fine years later, the risk stays.
And if you’re on allopurinol and have kidney disease, ask your doctor about testing for HLA-B*58:01. It’s a simple blood test. It could save your life.
Final Thoughts
DRESS syndrome is rare - only 1 in 1,000 to 1 in 10,000 drug exposures. But it’s deadly, often missed, and preventable. The key is knowing the warning signs and acting fast. It’s not about being paranoid. It’s about being informed. If you’re on a high-risk drug and feel off, trust your gut. Fever plus rash after weeks of medication? That’s not normal. Get checked. Your life might depend on it.
Can DRESS syndrome be cured?
Yes, DRESS syndrome can be reversed if caught early. Stopping the triggering drug and starting corticosteroids quickly leads to full recovery in most cases. However, some patients suffer lasting organ damage or develop autoimmune diseases later. There’s no single “cure,” but timely treatment prevents death and reduces long-term harm.
How long does DRESS syndrome last?
The acute phase usually lasts 2 to 6 weeks with treatment. Skin rash can take up to 4 weeks to fade. But recovery isn’t over then. Steroid tapering takes 4 to 8 weeks. Some patients experience fatigue or organ issues for months. Reactivation of HHV-6 can prolong symptoms. Full recovery may take 3 to 6 months.
Is DRESS syndrome hereditary?
DRESS itself isn’t inherited, but your genetic makeup can make you far more likely to develop it. The HLA-B*58:01 gene strongly increases risk for allopurinol-induced DRESS, especially in people of Asian descent. This gene is passed down, so if a close relative had a severe drug reaction, you may be at higher risk too.
Can you get DRESS from over-the-counter drugs?
Yes. While most cases come from prescription drugs like allopurinol or antiseizure meds, some OTC drugs have triggered DRESS. This includes certain herbal supplements and even some pain relievers containing sulfonamides. Always assume any new medication - even if bought without a prescription - could be a trigger.
What’s the difference between DRESS and a regular drug allergy?
A regular drug allergy causes symptoms like hives, swelling, or anaphylaxis within minutes to hours of taking the drug. DRESS takes weeks to develop and involves fever, eosinophilia, and damage to internal organs - not just the skin. It’s not an IgE-mediated reaction like typical allergies. It’s a delayed, complex immune response that affects the whole body.




14 Comments
DRESS is one of those conditions that should be taught in every med school curriculum. The delayed onset is what makes it so treacherous - patients and doctors alike assume it's a virus because it's been weeks. But that lag is the killer. I've seen two cases in my practice, both misdiagnosed for over a month. By then, liver enzymes were through the roof. Early detection saves lives, period.
Allopurinol kills more people than people think. If you have kidney issues and they give you allopurinol, walk out. Simple. No debate.
India needs to adopt HLA-B*58:01 testing like Taiwan - why are we still playing Russian roulette with gout meds? Our hospitals are full of patients who could’ve been saved with a $50 gene test. This isn’t science - it’s negligence.
Did you know the CDC has known about HHV-6 reactivation in DRESS since 2015? But pharma companies don’t want you to know - because if you knew, you’d stop taking these drugs. The real question is: who’s profiting from your slow poisoning?
This is exactly why we need better patient education. I’m a nurse and I’ve had patients come in with rashes, scared to say anything because they think their doctor will blame them. We need to normalize saying: ‘I’m on this med, I feel off - could it be DRESS?’ It’s not paranoia. It’s power.
I want to thank you for writing this. My sister had DRESS after taking lamotrigine. She was misdiagnosed for six weeks. By the time they figured it out, her liver was failing. She spent 56 days in the ICU. Now she has autoimmune thyroiditis and needs lifelong monitoring. I wish I’d known what to look for. This post could save someone’s life - thank you for sharing the details.
It is imperative to underscore that the pathophysiological underpinnings of DRESS syndrome represent a paradigmatic example of immune dysregulation, wherein the interplay between drug haptenization, T-cell clonal expansion, and cytokine storm cascades culminates in multi-organ failure. The diagnostic criteria, as outlined by the RegiSCAR group, remain the gold standard, yet clinical awareness remains woefully inadequate in primary care settings, particularly in resource-constrained environments where laboratory infrastructure is insufficient to detect eosinophilia or atypical lymphocytosis. Moreover, the delayed onset, often exceeding 14 days, creates a diagnostic blind spot that is exacerbated by the non-specificity of prodromal symptoms, which mimic infectious etiologies such as Epstein-Barr virus or cytomegalovirus. The imperative for preemptive HLA genotyping in high-risk populations cannot be overstated - it is not merely a diagnostic tool, but a prophylactic intervention of profound ethical and clinical significance.
Of course it’s dangerous - you’re letting Big Pharma push these drugs on people like candy. Why don’t they just make a safer version? Oh right - because they make more money off people dying. Wake up.
lol why are you all so scared of meds? I’ve been on carbamazepine for 12 years. No rash. No fever. No big deal. Stop fearmongering. This isn’t a horror movie.
It’s tragic how many people are willing to risk their lives for convenience. If you’re too lazy to get a genetic test before taking allopurinol, then you deserve what you get. This isn’t medical negligence - it’s personal irresponsibility.
I had DRESS after taking sulfamethoxazole... I cried for three days. My skin was burning, my eyes swelled shut, and I felt like my insides were melting. I still have nightmares. Now I carry a card in my wallet: ‘DO NOT GIVE ME SULFONAMIDES.’ I’m alive - but I’m not the same. 😢
Life is just a series of chemical reactions. Drugs are just molecules. Our bodies are just meat. DRESS? Just a glitch in the system. We’re all going to die anyway. Why stress over it?
Just to add another layer - I’ve been following the literature on anakinra for DRESS since the 2022 trial. The mechanism is fascinating: IL-1 blockade interrupts the cytokine cascade that’s driving the organ damage. But here’s what’s not talked about enough - the rebound effect after steroid taper. Some patients relapse when steroids are reduced too quickly, even if they’re off the trigger drug. That’s why we need longer monitoring periods. And honestly, I think we should be looking at JAK inhibitors next. The data on ruxolitinib in refractory cases is promising, though still anecdotal. We’re moving from reactive treatment to proactive immune modulation - it’s a new era.
As a doctor from Nigeria, I can tell you - we don’t even have eosinophil counters in 80% of our clinics. We see patients with rashes and fever, we give antibiotics, they die. No one even thinks of DRESS. This is a global issue, not just a Western one. We need mobile labs. We need training. We need help.