When your doctor orders liver function tests, it’s not because they think you’re sick. More often, it’s because something small - a weird feeling after eating, a blood test from a routine checkup, or even just your weight - made them pause. You get the results back and see numbers for ALT, AST, bilirubin, and ALP. You Google them. Suddenly, you’re scrolling through scary websites wondering if you have cirrhosis. The truth? Most of the time, you don’t. But understanding what these numbers mean can save you from unnecessary panic - or missed warning signs.
What Liver Function Tests Actually Measure
The term "liver function tests" is misleading. These aren’t tests that measure how well your liver is working, like a heart monitor measures pumping. They measure damage. When liver cells get injured, they leak enzymes and proteins into your blood. Those are what the tests catch.
The standard panel includes ALT (alanine aminotransferase), AST (aspartate aminotransferase), ALP (alkaline phosphatase), GGT (gamma-glutamyl transferase), bilirubin, albumin, and sometimes prothrombin time. But not all of them are equal. ALT and AST tell you about cell damage. Bilirubin and ALP tell you about bile flow. Albumin and prothrombin time tell you how well your liver is making proteins - that’s the only true "function" test here.
Reference ranges vary by lab, but typical values are: ALT 7-55 U/L, AST 8-48 U/L, total bilirubin 3-17 μmol/L, and albumin 35-50 g/L. These numbers aren’t magic. Normal doesn’t always mean healthy. And abnormal doesn’t always mean disease.
ALT and AST: The Liver’s Early Warning System
ALT is almost entirely in the liver. If it’s high, your liver is likely injured. AST is trickier. It’s in the liver, but also in your heart, muscles, and even red blood cells. That’s why a high AST alone could mean a heart attack, intense workout, or muscle injury - not liver trouble.
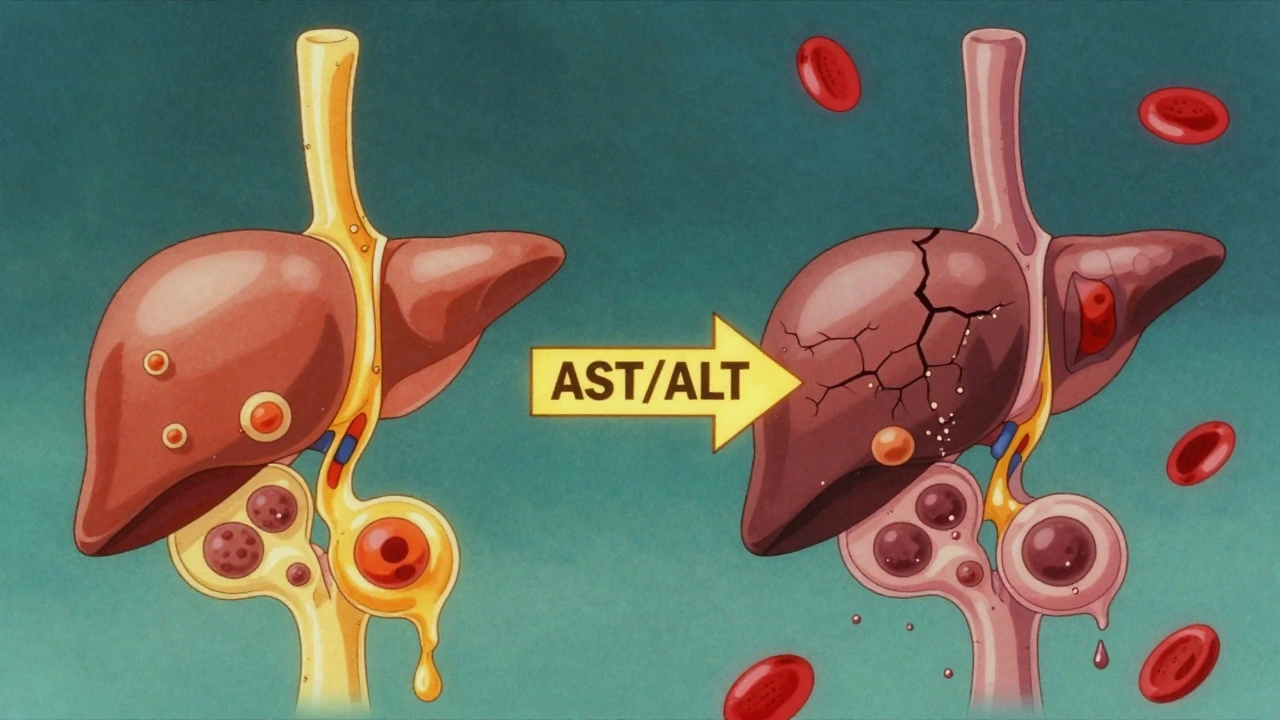
Here’s what matters: the ratio of AST to ALT.
- If AST is more than twice ALT - think alcohol. This pattern shows up in 90% of heavy drinkers with liver damage.
- If ALT is higher than AST - think fatty liver, hepatitis, or medication reactions. This is common in people with obesity or type 2 diabetes.
- If both are sky-high - over 1,000 U/L - that’s a red flag. It could be viral hepatitis, a drug overdose (like acetaminophen), or a sudden lack of blood flow to the liver.
ALT has a half-life of about 47 hours. That means if you stop drinking or stop taking a harmful drug, ALT will drop slowly over days. AST fades faster. So if your AST drops quickly but ALT stays high, your liver is still healing.
And here’s something most people don’t know: normal ALT levels are higher in men and in people with obesity. If your BMI is over 30, your "normal" ALT might be 10-15% higher than someone lean. That’s not disease - it’s biology.
Bilirubin: The Yellow Clue
Bilirubin is the waste product your liver clears from old red blood cells. When it builds up, your skin and eyes turn yellow - that’s jaundice. But you can have high bilirubin without looking yellow.
Bilirubin comes in two forms: unconjugated (before the liver processes it) and conjugated (after). A blood test usually gives you total bilirubin. If it’s high, your doctor will check the direct (conjugated) part.
- If conjugated bilirubin is high and ALP is also high - you have cholestasis. That means bile isn’t flowing. Causes: gallstones, tumors, or medication reactions.
- If unconjugated bilirubin is high and ALP is normal - it’s likely not liver-related. Think hemolysis (red blood cells breaking down too fast) or Gilbert’s syndrome - a harmless genetic condition that affects 5-10% of people.
ALP is another tricky marker. It’s made in the liver and bones. If ALP is high but GGT is normal, it’s probably not your liver. It could be a bone issue - like healing a fracture or Paget’s disease. That’s why doctors always check GGT with ALP. If both are up, it’s liver-related. If only ALP is up, look elsewhere.
Albumin and Prothrombin Time: The Real Liver Function Tests
These are the only tests that show whether your liver is still doing its job - making proteins and helping your blood clot.
Albumin is a protein your liver makes every day. It keeps fluid in your blood vessels. If albumin drops below 35 g/L, it means your liver has been damaged for months - maybe years. It doesn’t spike quickly. It’s a slow, steady decline. Low albumin often shows up in advanced cirrhosis.
Prothrombin time (PT) measures how long it takes your blood to clot. Your liver makes clotting factors. If PT is prolonged, your liver isn’t making them fast enough. This can happen in acute liver failure - like from a drug overdose - or in severe chronic disease.
Here’s the key difference: ALT and AST tell you about current damage. Albumin and PT tell you about long-term function. One is a siren. The other is a slow leak.
Patterns Matter More Than Single Numbers
A single high ALT doesn’t mean much. But a pattern? That’s gold.
- Hepatocellular pattern: ALT and AST way up, ALP and bilirubin normal or slightly up. This means liver cells are dying. Common causes: viral hepatitis, fatty liver, drug injury.
- Cholestatic pattern: ALP and bilirubin way up, ALT and AST only mildly elevated. This means bile flow is blocked. Common causes: gallstones, bile duct cancer, medication side effects.
- Mixed pattern: All markers elevated. This happens in drug-induced liver injury, autoimmune hepatitis, or advanced cirrhosis.
Doctors use ratios to spot these patterns fast. If ALT is more than 10 times the upper limit and ALP is less than 3 times, it’s hepatocellular. If ALP is more than 3 times and ALT is less than 10 times, it’s cholestatic.
And here’s what most people get wrong: mild elevations are common. About 10-15% of healthy people have ALT or AST slightly above normal - no disease, no risk. That’s why doctors don’t jump to scans or biopsies for ALT levels under 80 U/L. They wait. They ask about alcohol, medications, weight, and symptoms.
When to Worry - And When to Relax
Most people with mildly elevated liver enzymes never develop serious disease. But some patterns need action.
Worry if:
- ALT or AST is over 500 U/L - especially if it’s rising fast (more than 100 U/L per week).
- Bilirubin is over 50 μmol/L and you’re yellow.
- Albumin is below 30 g/L or PT is significantly prolonged.
- You have symptoms: swelling in your belly, dark urine, vomiting, confusion.
Relax if:
- Your ALT is 41-80 U/L and you have no symptoms, no alcohol use, no obesity.
- Your AST/ALT ratio is less than 1 and you’re otherwise healthy.
- Your bilirubin is slightly high but your ALP is normal - you might have Gilbert’s syndrome.
A 2021 study of over 12,000 people showed that combining LFT patterns with a simple score called FIB-4 (which uses age, platelets, AST, and ALT) improved diagnosis of advanced liver scarring from 68% to 89%. That’s huge. It means your doctor doesn’t need to order a biopsy right away - they can use blood tests to guess your risk.
What to Do Next
If your liver tests are off, don’t panic. Don’t Google. Don’t start detoxes or supplements. Do this:
- Look at your lifestyle. Are you drinking? How much? Are you taking OTC painkillers like acetaminophen? Are you gaining weight?
- Ask your doctor: "Is this a new change?" If your last test was normal six months ago, that’s more concerning than if it’s been high for years.
- Ask: "Should we check for fatty liver?" It’s the most common cause of elevated liver enzymes in people under 50.
- Ask: "Should we do FIB-4?" It’s free, simple, and tells you if you’re at risk for scarring.
- Don’t get a scan unless your doctor recommends it. Most mild elevations don’t need imaging.
And if you’re overweight? Losing 5-10% of your body weight can drop ALT levels by 40% or more. That’s more effective than any supplement.
There’s a new term now: MASLD - Metabolic Dysfunction-Associated Steatotic Liver Disease. It’s what doctors used to call NAFLD. The name changed because it’s not just "fatty" - it’s about how your body uses sugar and fat. And it’s the #1 reason for elevated liver enzymes today.
What’s Coming Next
Doctors are moving beyond just ALT and AST. New blood tests like the ELF test (Enhanced Liver Fibrosis) can detect early scarring before it shows up on ultrasound. These tests are already being used in clinics in Canada and Europe. They’re not perfect, but they’re better than guessing.
The future of liver health isn’t about more tests. It’s about knowing which ones matter - and when to stop testing.





9 Comments
Man, I remember when my ALT was through the roof and I thought I was one beer away from a liver transplant. Turned out I was just taking ibuprofen like candy and had gained 20 lbs from lockdown pizza. Cut out the junk, lost the weight, and my numbers went back to normal in 4 months. No meds, no magic pills - just real life changes. Don’t panic, just adjust.
Also, Gilbert’s syndrome is way more common than people think. I’ve got it. My bilirubin spikes when I’m stressed or skip breakfast. I look like a jaundiced ghost on Mondays, but I’m fine. Docs just shrugged and said, 'You’re one of those weirdos who’s healthy but looks sick.'
Stop Googling. Start living.
It is imperative to underscore the clinical significance of the hepatocellular versus cholestatic patterns delineated in this exposition. The diagnostic utility of the AST:ALT ratio, particularly in the context of alcoholic liver disease, remains a cornerstone of biochemical hepatology. Furthermore, the incorporation of FIB-4 as a non-invasive fibrosis screening tool represents a paradigm shift in primary care management of metabolic dysfunction-associated steatotic liver disease (MASLD).
It is also noteworthy that the reference ranges for ALT are population-dependent, with higher thresholds observed in male subjects and those with elevated BMI. This necessitates individualized interpretation rather than reliance on absolute normative values. The concomitant assessment of GGT with ALP remains indispensable for the exclusion of extrahepatic etiologies.
Further validation of ELF testing in diverse cohorts is warranted, though preliminary data suggest superior sensitivity in early fibrosis detection compared to transient elastography in certain subpopulations.
People these days just eat garbage and then act shocked when their liver goes bad. No one takes responsibility anymore. You drink, you eat sugar, you sit all day - and then you freak out because your ALT is 70? That’s not a medical mystery, that’s just consequences.
My cousin did the same thing. Lost 30 lbs, stopped soda, started walking. His ALT dropped to 28. No big deal. But he had to actually change. Not some detox tea. Real life. You want health? Work for it.
bro i just checked my last bloodwork and my AST is 52 😭
im gonna die right?
im 24 and i ate a burrito last night
send help
I’ve been reading this over and over because I’ve had mildly elevated ALT for like three years now and I’m still not sure what to think. I’m not an alcoholic, I don’t take anything crazy, I’m not obese - just a little overweight, maybe BMI 27. I’ve had two ultrasounds, both said ‘mild fatty infiltration’ - no fibrosis, no inflammation.
My doctor said, ‘Keep doing what you’re doing,’ and I’ve been walking 45 minutes a day, cutting back on processed stuff, and drinking more water. My ALT went from 68 to 54 over a year. It’s slow, but it’s moving. I think the key is not chasing perfect numbers, but just being consistent with small things.
Also, I didn’t know about Gilbert’s syndrome until I read this. My bilirubin’s always been a little high. I used to think I was sick. Turns out I’m just… weirdly built. That’s kinda comforting.
It’s weird how much anxiety these numbers cause. Like, I’ve had worse things happen in life - broken bones, bad breakups - but a single lab value makes me feel like I’m dying. Maybe we need better education on this stuff. Or at least, less scary Google results.
Let me be blunt: this article is dangerously naive. You say ‘don’t panic’ - but you’re ignoring the silent progression of fibrosis. The liver doesn’t scream until it’s too late. And FIB-4? It’s a statistical approximation - not a diagnostic tool. Many patients with normal FIB-4 have advanced scarring. Many with high FIB-4 are perfectly healthy.
And let’s not pretend that ‘losing 5-10% body weight’ is a cure-all. What if you’re already lean? What if you have NAFLD despite being athletic? What if your liver is damaged by environmental toxins - pesticides, plasticizers, mold exposure? No one talks about that.
This is the same lazy, reductionist medicine that tells people to ‘just eat less’ while ignoring systemic metabolic disruption. The real epidemic isn’t obesity - it’s the industrial food system. And until we address that, we’re just rearranging deck chairs on the Titanic.
ALERT: THE PHARMA INDUSTRY IS USING THIS TO SELL YOU LIVER “TESTS” AND “SUPPLEMENTS” TO KEEP YOU SCARED AND SPENDING! THEY DON’T WANT YOU TO KNOW THAT ALTERNATIVE LIVER DETOXES - LIKE DILUTED APPLE CIDER VINEGAR + CAYENNE PEPPER - CAN LOWER ALT IN 72 HOURS! THEY’RE HIDING THE TRUTH! THE FDA IS IN BED WITH BIG PHARMA! I’VE SEEN 17 CASES WHERE PEOPLE CURED THEIR LIVER WITH JUST WATER AND SUNLIGHT! WHY WON’T YOUR DOCTOR TELL YOU THIS?!?!?!!?!
my doc said my alt was 65 and i was like oh no but then i realized i was taking tylenol every day for my back pain and i was like wait a sec… i stopped and 2 months later it was 32. so yeah. dont ignore it but also dont freak out. just fix the simple stuff first. also i think they spelled fatty liver wrong. its not masld its just fat liver. why do they make it sound so fancy?
I want to thank you for writing this. I’ve been a nurse for 18 years, and I’ve seen so many patients - especially women over 40 - terrified by their liver results. They come in with printouts from WebMD, eyes wide, trembling. They’ve already decided they have cirrhosis.
This article doesn’t just explain the numbers - it gives people back their peace. That’s rare.
I’ve had patients who cut out soda, started walking after dinner, and stopped taking OTC painkillers without even realizing how much damage they were doing. Their numbers didn’t just improve - their energy, their sleep, their mood improved too. It’s not about fixing a lab value. It’s about fixing your relationship with your body.
And yes - Gilbert’s syndrome is real, it’s common, and it’s not a disease. I tell my patients: ‘You’re not broken. You’re just built differently.’ That changes everything.
If you’re reading this and you’re scared - breathe. You’re not alone. And you’re not doomed. Just take one small step. Maybe today, you’ll drink water instead of soda. That’s enough.