Tonsillitis-Induced Acid Reflux Checker
Assess Your Symptoms
Answer these questions to determine if your symptoms might be caused by tonsillitis-induced acid reflux.
Risk Assessment
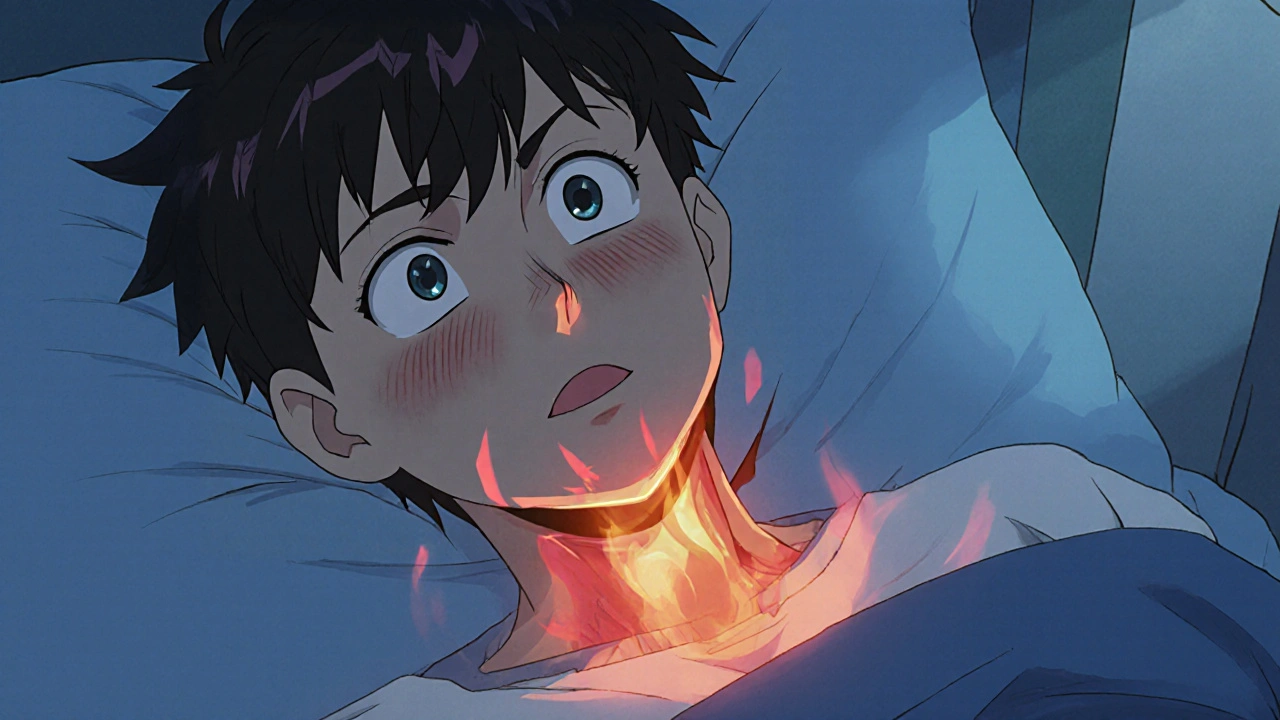
Ever wonder why a sore throat sometimes feels like a burn in your chest? That’s not a coincidence. Tonsillitis is a swollen, inflamed set of lymph nodes at the back of your throat, and it can set off a chain reaction that leads to acid reflux. In this guide we’ll break down the connection, spot the overlapping signs, and give you practical steps to keep both problems under control.
What’s Really Happening? The Anatomy Behind the Link
When your tonsils fight off bacteria or viruses, they release inflammatory chemicals like histamine, a molecule that widens blood vessels and makes tissues swell. That swelling can narrow the airway and push the tongue backward, especially when you’re lying down. The forced position pressures the lower esophageal sphincterthe muscular ring that keeps stomach acid from climbing back up the esophagus. A weak or mis‑aligned sphincter lets acid splash into the throat, creating the classic “heartburn” feeling.
In addition, the throat’s lining becomes more sensitive after a bout of tonsillitis. Even a tiny amount of acid can trigger a burning sensation, a cough, or a hoarse voice-symptoms that many people mistakenly attribute solely to the infection.
Common Overlap: Symptoms That Blur the Lines
Both conditions share a handful of red flags. Spotting them early can save you a trip to the ER and a mountain of medication.
| Symptom | Typical of Tonsillitis | Typical of Acid Reflux |
|---|---|---|
| Sore throat | ✔️ | ⚪ (may appear if acid reaches the throat) |
| Difficulty swallowing | ✔️ | ⚪ (can happen with severe reflux) |
| Hoarseness | ✔️ | ✔️ (laryngeal reflux) |
| Heartburn / Burning behind breastbone | ⚪ | ✔️ |
| Chronic cough | ⚪ | ✔️ |
Notice the “hoarseness” row? That’s a classic example of laryngeal refluxacid that reaches the voice box, irritating the vocal cords. If you’ve had tonsillitis and start losing your voice, it’s worth checking whether reflux is joining the party.
Diagnosing the Double Trouble
Doctors use a blend of visual exams and simple tests. A throat swab confirms a bacterial cause of tonsillitis, while an endoscopya thin camera that looks inside the esophagus and stomach can reveal acid damage. If you can’t get an endoscopy right away, a 24‑hour pH monitor (tiny sensor that measures acid levels) is a reliable alternative.
Blood work isn’t a primary tool for either condition, but a high white‑blood‑cell count may point to bacterial tonsillitis, guiding the doctor toward antibiotics.

Quick Lifestyle Tweaks That Hit Both Problems
- Elevate the head of your bed 6‑8 inches. Gravity keeps both the throat clear and stomach acid down.
- Avoid large meals within three hours of bedtime. Smaller, frequent meals reduce pressure on the esophageal sphincter.
- Limit trigger foods: citrus, tomato sauce, chocolate, caffeine, and spicy dishes can aggravate reflux and irritate inflamed tonsils.
- Stay hydrated, but sip water rather than gulp. Hydration thins mucus and helps neutralize acid.
- Quit smoking. Nicotine relaxes the sphincter and slows healing of tonsil tissue.
These changes don’t replace medical care, but they often shrink the severity of both conditions enough to speed up recovery.
Medical Options: When Home Remedies Aren’t Enough
If symptoms linger beyond a week, it’s time to talk to a clinician.
For bacterial tonsillitis, a short course of antibioticssuch as amoxicillin, which target streptococcal infection is standard. Viral cases resolve on their own, so doctors may simply recommend rest, throat lozenges, and fluids.
Acid reflux treatment starts with over‑the‑counter antacids, H2 blockers (like ranitidine), or proton‑pump inhibitors (PPIs) for more persistent cases. If you have a hiatal hernia-where part of the stomach pushes through the diaphragm-a surgical consultation might be on the table.
Speaking of surgery, for chronic tonsillitis that keeps sparking reflux, an tonsillectomyremoval of the tonsils, often performed under general anesthesia can break the cycle. The decision hinges on frequency of infections, severity of symptoms, and overall health.
Another supportive avenue is gut health. Probiotics (probioticsbeneficial bacteria that help balance the gastrointestinal tract) may improve digestion and lower reflux episodes, especially after a course of antibiotics.

Red Flags: When to Call the Doctor Right Away
- Difficulty breathing or swallowing solid foods
- Severe, unrelenting chest pain (could mimic a heart attack)
- Fever over 101°F (38.3°C) lasting more than two days
- Persistent hoarseness lasting more than three weeks
- Vomiting blood or black, tarry stools (signs of bleeding)
These symptoms suggest complications that need prompt attention-such as peritonsillar abscess, esophageal erosion, or even Barrett’s esophagus.
Quick Checklist: Managing Tonsillitis‑Induced Reflux
- Raise your head while sleeping.
- Stick to small, low‑acid meals.
- Avoid smoking and alcohol.
- Use OTC antacids if heartburn appears.
- Contact a doctor if pain worsens after 7 days.
Frequently Asked Questions
Can tonsillitis cause permanent acid reflux?
Occasionally, chronic inflammation can weaken the lower esophageal sphincter, making reflux more likely. However, with proper treatment of the infection and lifestyle changes, most people see the reflux subside.
Do I need antibiotics for every case of tonsillitis?
No. Only bacterial tonsillitis, usually confirmed by a rapid strep test, requires antibiotics. Viral infections heal on their own.
Is a tonsillectomy ever recommended because of reflux?
It’s rare, but if tonsillitis repeatedly triggers severe reflux that doesn’t improve with medication, doctors may consider removal to break the cycle.
Can I use natural remedies for reflux while treating tonsillitis?
Yes. Herbal teas (like ginger), aloe vera juice, and chewing sugar‑free gum can boost saliva, which neutralizes acid. Just ensure they don’t irritate the sore throat.
What role does a hiatal hernia play in this combo?
A hiatal hernia pushes part of the stomach up through the diaphragm, making the lower esophageal sphincter less effective. This can amplify reflux symptoms that already flare up during a tonsillitis episode.





14 Comments
Wow, the link between tonsillitis and reflux is something most people never consider, and it really makes you think about how interconnected our bodies are. When the tonsils swell, the airway can get cramped, and that shift can push the tongue back, which in turn puts pressure on the lower esophageal sphincter. It's like a domino effect that you wouldn't expect from a simple sore throat. The inflammation releases histamine, which not only makes the tissue swell but also sensitizes the lining of the throat to even a tiny amount of acid. That explains why a mild heartburn can feel like a blazing fire after a bout of tonsillitis. I also appreciate the practical tips about elevating the head of the bed; gravity really is a simple yet powerful ally. Small, low‑acid meals are another great suggestion-big meals before bed are a recipe for disaster for anyone dealing with reflux. Staying hydrated but sipping rather than gulping helps thin mucus and buffer acid, which is something I wish more people knew. Quitting smoking is a no‑brainer, since nicotine relaxes the sphincter and hampers healing. The article correctly points out that antibiotics are only for bacterial infections, which avoids unnecessary medication. For viral cases, rest and soothing lozenges do the trick, and you don't want to over‑medicate. Probiotics after antibiotics can help restore gut flora and may reduce reflux episodes, a nice bonus. If symptoms persist beyond a week, seeing a doctor is crucial to rule out complications like peritonsillar abscess or esophageal erosion. The red flag list is thorough, reminding us not to ignore severe chest pain or persistent hoarseness. Overall, this guide balances medical insight with everyday lifestyle tweaks, making it a useful resource for anyone dealing with these overlapping issues.
Totally agree, those bed‑elevating hacks are clutch. I tried a couple of inches and woke up feeling way better.
Nice rundown! The idea that a swollen tonsil can literally nudge the tongue and stress the LES is something I hadn't heard before. Keep those simple changes in mind-especially the food timing-because it’s easy to forget.
Honestly, people need to take responsibility for their health and not just ignore the signs. If you’re coughing and your throat hurts, it’s not just a cold; it could be the start of a bigger problem like reflux. Ignoring it is laziness, and it leads to more serious issues down the line.
Yo, stop sugarcoatin' it. People act like a sore throat is no big deal, but it’s a clear sign ur body’s fightin' somethin' nasty. You gotta dip the meds, stop the junk food, and quit that smokes-otherwise u’ll be stuck with that burn forever.
From a philosophical standpoint, this article reminds us how the micro‑cosm of an inflamed tonsil reflects the macro‑cosm of our overall health. The chain reaction from local inflammation to systemic reflux illustrates the principle of interdependence. It's a beautiful, albeit painful, demonstration of how one small disturbance can ripple through the whole system.
Ah, the classic over‑medicalization. As if everyone needs a fancy endoscopy for a sore throat that could be cured by wiping your mouth. Some people just love turning simple issues into high‑tech drama.
While the clinical details are accurate, the article could benefit from a more nuanced discussion of the differential diagnosis. For instance, distinguishing laryngeal reflux from purely infectious causes requires careful laryngoscopic evaluation, which is not mentioned here.
Thank you for your thoughtful observation. Indeed, a comprehensive assessment that includes laryngoscopy can clarify the underlying etiology and guide appropriate management.
Love the energy! A splash of ginger tea, a dash of colorful veggies, and you’ve got a tasty antidote to both irritation and acid. Keep the creative tweaks coming!
Absolutely! It’s fascinating how a simple change in diet can ripple into both oral and gastrointestinal health. I’ve experimented with mindful eating and have seen real improvements in my own throat comfort.
Wow-who knew a sore throat could double as a fire alarm for your chest?
Exactly, and the fix isn’t rocket science-just lift that pillow and cut the junk. No need for drama, just do it.
Well, if you’d actually read the article instead of scrolling endlessly, you’d realize that the “miraculous” cure is simply basic physiology. No need for conspiracy theories-just follow the evidence.