Every year, millions of people take multiple medications - often mixing brand-name drugs with cheaper generics. What most don’t realize is that generic drug interactions can be just as dangerous as those between brand-name drugs. A pill you picked up at your local pharmacy might seem harmless, but when combined with your blood pressure med or your daily aspirin, it could trigger a serious reaction. That’s where digital consultation tools come in - not as fancy gadgets, but as essential safety nets for anyone managing more than a few prescriptions.
Why Generic Drugs Aren’t Always Safe Together
Generic drugs are chemically identical to their brand-name versions. That’s the law. But here’s the catch: just because two drugs are generics doesn’t mean they play nice together. Take a common combo: a generic statin like atorvastatin and a generic antibiotic like clarithromycin. On paper, both are safe alone. Together, they can spike your muscle enzyme levels so high that you risk rhabdomyolysis - a condition that can damage your kidneys. This isn’t rare. The Journal of the American Medical Association found the average person over 65 takes 4.8 prescriptions at once. More drugs = more chances for something to go wrong.What Digital Consultation Tools Actually Do
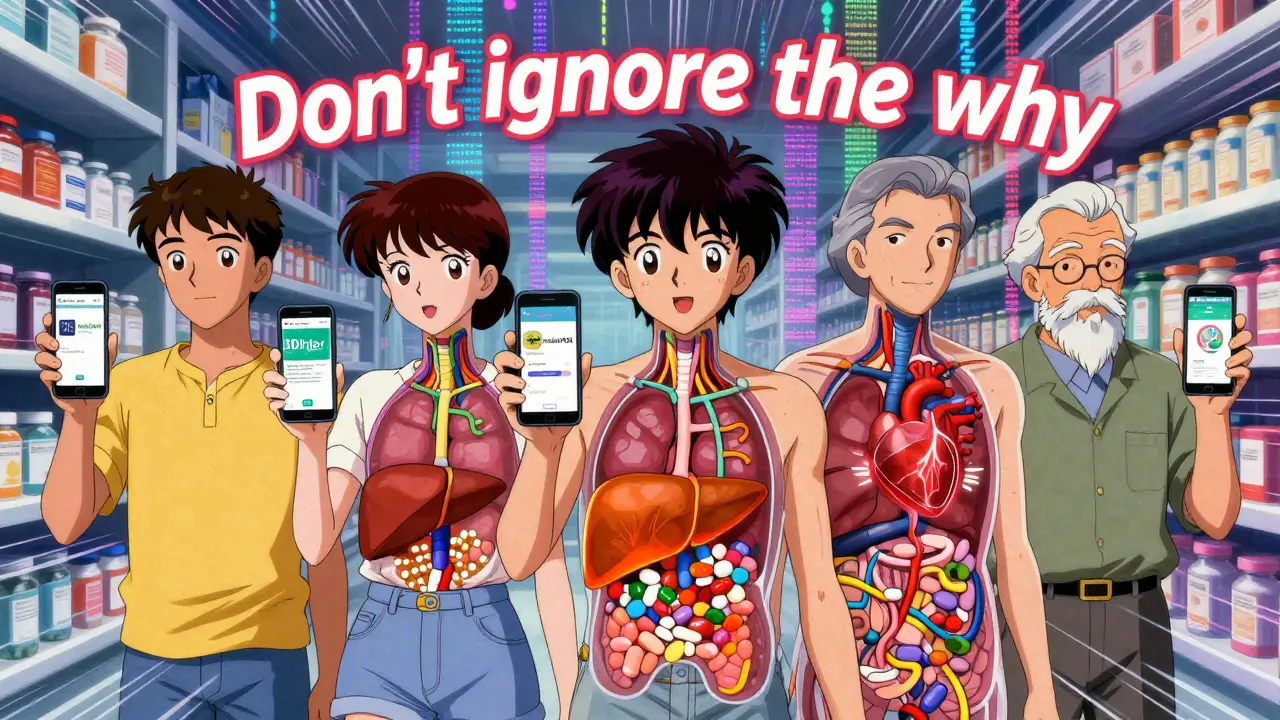
These aren’t just apps that tell you if two drugs “might interact.” They’re clinical decision engines trained on real-world data. Tools like Epocrates, Micromedex, and DDInter scan your list of medications - brand, generic, even supplements - and match them against databases of known interactions. They don’t just say “warning.” They tell you why: is it a metabolic conflict? A blood pressure spike? A serotonin overload? They grade severity: mild, moderate, severe. And some even flag if a drug’s effect is reduced - meaning your painkiller isn’t working because something else is blocking it.Top Tools Compared: What Works Best for You
| Tool | Max Drugs Checked | Free Access? | Overdose Info? | Best For |
|---|---|---|---|---|
| Epocrates | 30 | Yes (robust free version) | No | Outpatients, quick checks, herbal supplements |
| Micromedex | Unlimited (enterprise) | No (paid only) | No | Hospitals, IV compatibility, complex regimens |
| UpToDate Lexidrug | 50+ | Partially (subscription) | Yes | Clinicians needing overdose reversal protocols |
| DDInter | 5 | Yes (no login) | No | Researchers, academic use, detailed mechanisms |
| mobilePDR | 10 | Yes (limited) | No | Users wanting manufacturer-updated summaries |
Epocrates stands out for everyday users. It’s the only tool that lets you check 30 drugs at once - including herbal supplements like St. John’s Wort or turmeric - without paying a cent. That’s huge. A lot of people don’t think of supplements as drugs, but they’re often the hidden cause of interactions. One patient I know started taking garlic pills for cholesterol and ended up in the ER because they clashed with his warfarin. Epocrates flagged it instantly.
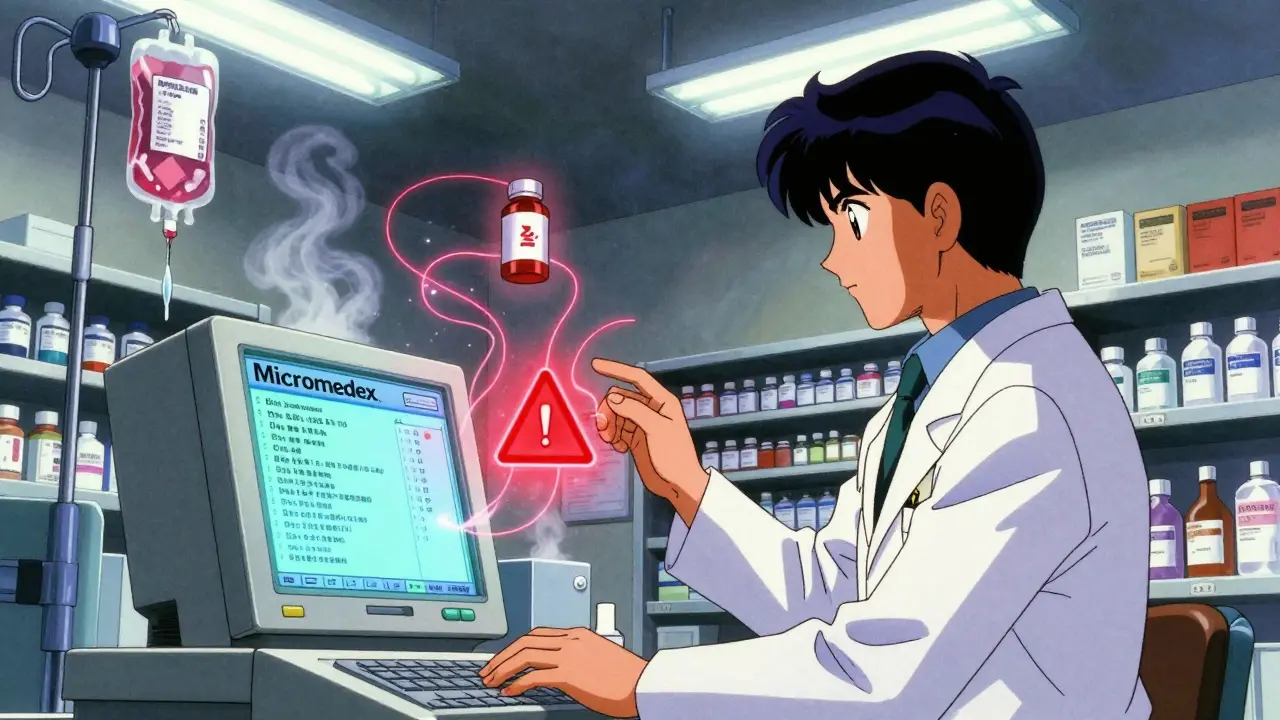
Micromedex is the workhorse in hospitals. It’s not for casual use. It’s for pharmacists managing 10+ meds for ICU patients. It checks IV compatibility - something no other app does well. If you’re on a drip of vancomycin and your nurse adds a new antibiotic, Micromedex tells you if they’ll cloud up in the line. That’s life-or-death stuff.
UpToDate Lexidrug is the only one that tells you what to do if someone overdoses. Not just “this is dangerous” - but “give them naloxone,” “start activated charcoal,” “monitor for QT prolongation.” That’s rare. Only Drugs.com matches it.
The Hidden Problem: Too Many Alerts
Here’s the ugly truth: these tools are smart, but they’re not perfect. A 2023 JAMA Internal Medicine study found that clinicians ignore 49% to 96% of interaction warnings - not because they’re careless, but because the systems flood them with false alarms. A tool might flag a mild interaction between two common drugs that have been safely used together for decades. After seeing 20 of these a day, doctors start tuning them out. That’s called alert fatigue. And when you tune out, you miss the real danger.That’s why customization matters. Hospitals using Micromedex now let their teams set severity thresholds. If you’re a 70-year-old with kidney disease, you get flagged for everything. If you’re a healthy 30-year-old, you only get the red flags. That cut false alerts by 40% in one 2023 trial.
What’s New in 2026
The field is moving fast. In January 2024, DDInter rolled out Version 2.0 with machine learning that predicts interactions not yet documented - like how a new generic antifungal might affect a common antidepressant. Merative, the company behind Micromedex, bought a startup called InteracDx in late 2023 to do the same. Their goal? Reduce false positives by 35% by 2026. The FDA has also made improving these algorithms a top priority in its Digital Health Innovation Plan.That means the tools aren’t just reacting anymore - they’re anticipating. They’re learning from millions of real patient records to spot patterns no human could catch. One study showed AI-enhanced systems caught 22% more high-risk interactions than older versions.
How to Use These Tools Right
You don’t need to be a doctor to use them. Here’s how to make them work for you:- Keep a real-time list - Write down every pill, patch, and supplement you take. Include doses and frequency. Don’t rely on memory.
- Check before you start anything new - Even if your doctor prescribes it, run it through Epocrates or DDInter yourself. Ask: “Is this safe with my other meds?”
- Don’t ignore the “why” - If it says “increased bleeding risk,” don’t just click past. Look up what that means. Is it your blood thinner? Your fish oil? Your NSAID?
- Ask your pharmacist - They have access to Micromedex and UpToDate. Don’t be shy. Say: “Can you run this combo through your system?”
- Update regularly - New interactions pop up every week. Recheck your list every 3 months or after any new prescription.
What You Shouldn’t Do
- Don’t assume generics are always safe together. Just because they’re cheap doesn’t mean they’re low-risk.
- Don’t trust free apps that don’t cite sources. If it doesn’t mention DrugBank, Micromedex, or FDA data, it’s not reliable.
- Don’t skip checking supplements. Green tea extract, ginkgo, and even vitamin K can interfere with your meds.
- Don’t wait for symptoms. Many interactions cause no warning signs until it’s too late.
Final Thought: Tools Don’t Replace Knowledge - They Extend It
Digital consultation tools aren’t magic. They won’t tell you if your headache is from stress or a drug clash. But they’ll tell you if the combination you’re taking could be the reason. In a world where polypharmacy is the norm, not the exception, these tools are the closest thing we have to a safety net. Use them. Update them. Share them with your family. Because when it comes to your meds, ignorance isn’t bliss - it’s a risk you don’t need to take.Are generic drugs more likely to cause interactions than brand-name drugs?
No. Generic drugs contain the same active ingredients as brand-name versions, so their interaction profiles are identical. The risk comes from combining multiple drugs - generic or brand - not from whether they’re generic. What changes is cost, not chemistry.
Can I use these tools if I’m not a healthcare professional?
Yes. Epocrates and DDInter are free and designed for patients and caregivers. You don’t need a license. Just enter your meds, and the tool will show you potential risks. If you see a red flag, take it to your doctor or pharmacist - don’t stop your meds on your own.
Why does Epocrates let me check 30 drugs but DDInter only 5?
Epocrates is built for busy clinicians who need to check full medication lists quickly - like during a 10-minute office visit. DDInter was designed as a research tool for scientists studying interaction patterns. It’s more detailed but slower. If you’re managing your own meds, Epocrates is the practical choice.
Do these tools work with over-the-counter meds and supplements?
Yes - but only some do it well. Epocrates has the most comprehensive database for OTCs and supplements. DDInter and mobilePDR include some, but not all. If you take melatonin, ginger, or fish oil, make sure your tool lists them. Many free tools ignore supplements entirely.
Is it worth paying for Micromedex or UpToDate?
Only if you’re a healthcare provider managing complex cases - like someone on 8+ medications, with kidney or liver disease, or in a hospital setting. For personal use, Epocrates is free and powerful enough. Paying for Micromedex as a patient is like buying a surgical scalpel to open a jar.
How often are these tools updated?
Top tools update within days of new FDA warnings or drug label changes. mobilePDR guarantees updates within a week of manufacturer changes. Epocrates and Micromedex update continuously. DDInter updates monthly. If a new interaction is published in a medical journal, it usually shows up in these tools within 30 days.
Next Steps: What to Do Today
1. Open your medicine cabinet. Write down every pill, patch, and bottle you take - even the ones you only use once a month.2. Download Epocrates (free on iOS and Android). Enter your list.
3. Look at the results. If anything says “severe” or “contraindicated,” don’t panic. But do call your pharmacist and say: “I saw this warning. Can we talk about it?”
4. Set a calendar reminder to check your list again in 90 days. Medications change. So should your safety plan.





8 Comments
Just downloaded Epocrates after reading this. Been taking turmeric and blood pressure meds for years-never thought they’d clash. Turned out it flagged a moderate interaction. Called my pharmacist today and we swapped one of my pills. Feels good to actually be proactive instead of just hoping for the best.
Also, shoutout to the author-this is the kind of stuff that actually saves lives. Not just fluff.
Man, in India we just grab generics off the shelf like candy. No one checks anything. My uncle took statin + clarithromycin for a cold and ended up in the hospital with muscle pain. Took them months to figure out why. This post? Pure gold. Should be mandatory reading before you buy any pill that isn’t paracetamol.
While I appreciate the pragmatic tone, one must acknowledge the inherent epistemological limitations of consumer-facing pharmacovigilance platforms. The clinical decision support systems referenced, while statistically robust, remain fundamentally reactive architectures predicated on retrospective pharmacokinetic datasets. The emergent machine learning models, such as those deployed by InteracDx, represent a paradigmatic shift toward predictive modeling-but until they are validated against prospective, longitudinal cohort studies with ethnographically diverse populations, their clinical utility remains probabilistic rather than deterministic.
Moreover, the normalization of patient self-diagnosis via mobile applications risks exacerbating iatrogenic harm through confirmation bias and therapeutic misalignment. One must ask: is accessibility synonymous with safety?
Look, I get the jargon-heavy folks love to overcomplicate things, but here’s the real deal: if you’re on more than three meds, you’re playing Russian roulette with your kidneys. Epocrates is free, works offline, and checks supplements too. No excuse not to use it.
I’m a nurse. I’ve seen people ignore warnings until they’re in the ER with creatinine levels through the roof. Just open the app. Type in your pills. If it says ‘severe,’ don’t Google it-call your pharmacist. Done. No drama. Just save your life.
How quaint. A blog post masquerading as medical authority, complete with a table that barely scratches the surface of pharmacodynamic complexity. One must wonder if the author has ever reviewed a true drug interaction profile from the FDA’s FAERS database-or merely skimmed a marketing brochure from Epocrates’ corporate sponsors.
And to suggest that supplements are ‘hidden causes’? How pedestrian. The real issue is the erosion of clinical judgment in favor of algorithmic crutches. I’ve seen patients refuse life-saving antibiotics because an app flagged a ‘moderate’ interaction with green tea. The irony is not lost on those of us who trained before smartphones became de facto pharmacists.
Epocrates? In America? Please. We have the most advanced healthcare system in the world. Why are we using some free app built by a grad student? Micromedex is the gold standard-and if you can’t afford it, you shouldn’t be managing your own meds. This whole ‘patient empowerment’ nonsense is just a cover for lazy doctors and overworked pharmacists offloading responsibility. If you can’t pay for proper care, maybe you shouldn’t be taking five pills a day.
You know, it’s interesting how everyone’s so quick to praise these apps without ever asking who built them, or what data they’re trained on, or whether the companies behind them have ever been fined for misleading claims. I’ve seen DDInter’s source code-well, the public version-and it’s barely more than a regex matcher with a pretty UI. The real work? Done by pharmacists in hospital backrooms, updating databases manually because the algorithms still can’t distinguish between a drug interaction and a coincidental lab result.
And yet we’re told to trust this? To rely on a free app that doesn’t even know if you’re fasting or drinking grapefruit juice? It’s not just naive-it’s dangerously complacent. The system is broken, and no app can patch a leak this big.
Just wanted to say thanks for writing this. I’m 72, on six meds, and my grandkids helped me download Epocrates last week. We checked everything-my fish oil, my melatonin, even the ginger chews I take for nausea. Turned out one of my blood pressure pills was canceling out the other. We called my doc, adjusted the dose, and now I’m sleeping better than I have in years.
It’s not about tech replacing people. It’s about tech helping people help themselves. And that’s worth something.