When you’ve had a serious reaction to a medication-hives, swelling, trouble breathing, or worse-it’s natural to assume you’ll never be able to take that drug again. But what if that drug is the only one that can save your life? For people with cancer, autoimmune diseases, or chronic infections, stopping a life-saving medication isn’t an option. That’s where drug desensitization comes in.
What Is Drug Desensitization?
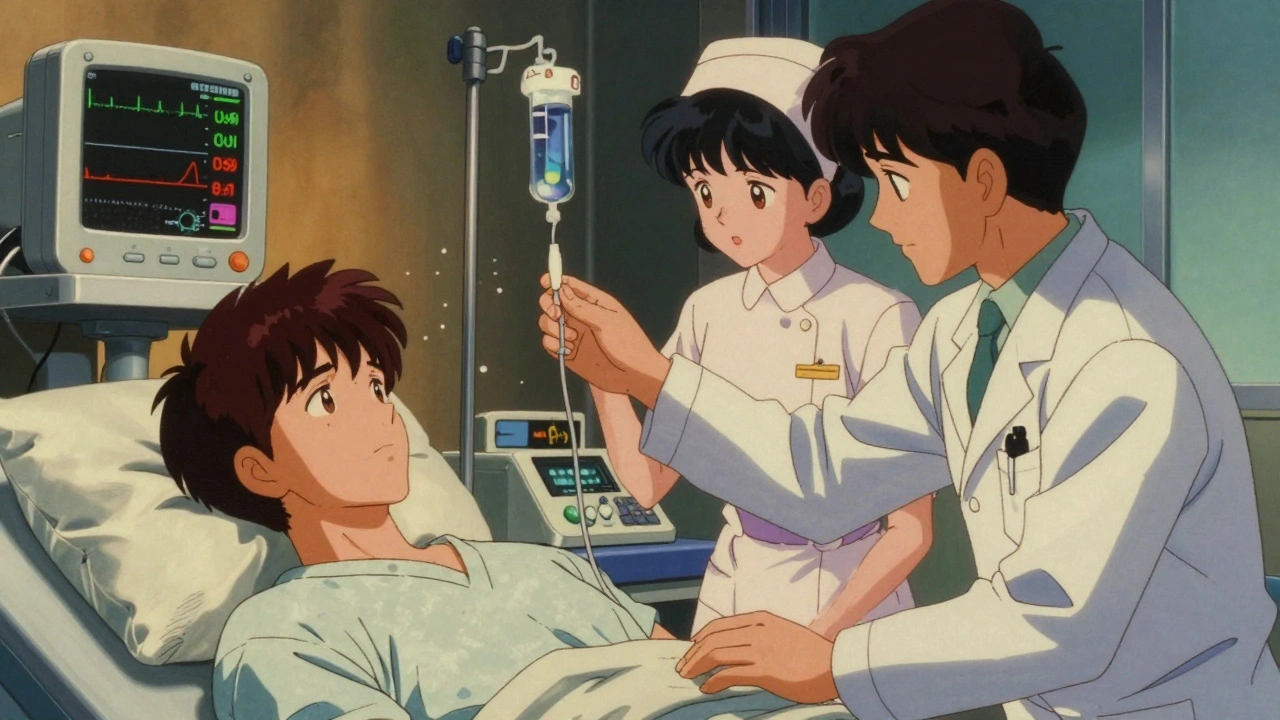
Drug desensitization is a controlled, step-by-step process that lets your body temporarily tolerate a medication you’re allergic to. It’s not a cure. It doesn’t change your immune system permanently. But it gives you a window-hours or days-to receive the full dose of the drug you need without triggering a dangerous reaction. This isn’t something you try at home. It’s done only in a hospital or specialized clinic, under constant medical supervision. Every step is planned, monitored, and ready to be stopped if needed. The goal? Get you to the full therapeutic dose safely, so treatment can continue.Who Needs It?
Not everyone with a drug allergy qualifies. Desensitization is reserved for cases where:- There’s no safe alternative drug available
- The drug is critical-like chemotherapy, antibiotics for cystic fibrosis, or biologics for rheumatoid arthritis
- You’ve had a confirmed IgE-mediated reaction (like anaphylaxis, hives, or swelling)
- Antibiotics (penicillin, vancomycin, carbapenems)
- Chemotherapy drugs (platinum-based agents, taxanes)
- Monoclonal antibodies (rituximab, infliximab, cetuximab)
- Aspirin and NSAIDs (even though these reactions aren’t always IgE-mediated)
- Local anesthetics
- Iron infusions
How It Works: The Protocol
There’s no one-size-fits-all plan. Each protocol is customized based on the drug, your reaction history, and your overall health. But most follow a similar pattern. For intravenous drugs (like antibiotics or chemo), the standard is a 12-step or 16-step process. You start with a tiny fraction of the full dose-often 1/10,000th-and gradually double it every 15 to 30 minutes. Each step is followed by close monitoring:- Blood pressure checked every 5 minutes
- Oxygen levels tracked with pulse oximetry
- Heart rate and breathing monitored
- Spirometry for patients with asthma
- Physical exam before each dose
What Happens If You React?
Reactions during desensitization aren’t rare-but they’re expected and managed. If you develop itching, hives, wheezing, or a drop in blood pressure, the team doesn’t panic. They pause, assess, and adjust. Common adjustments include:- Slowing down the dose increases
- Going back to the last dose you tolerated
- Adding antihistamines or steroids before continuing
- Extending the time between doses to 45 or 60 minutes

What’s Not Safe?
Desensitization is powerful-but it’s not for everyone. It’s strictly avoided in people who’ve had:- Stevens-Johnson syndrome
- Toxic epidermal necrolysis
- Erythema multiforme with blistering
- Drug-induced hepatitis or nephritis
- Serum sickness reactions
Why It Works (And Why It’s Temporary)
The science behind desensitization isn’t fully understood, but it likely involves temporarily turning down your immune system’s alarm system. Your mast cells-responsible for releasing histamine during allergic reactions-become less reactive after repeated, low-dose exposure. The key word here is temporary. Once you stop taking the drug for more than a few days, your allergy can come back. That’s why:- If you miss a dose by more than 12-24 hours, you may need to restart the entire process
- For chronic conditions (like rheumatoid arthritis), you might need daily desensitization just to keep taking your biologic
- Even after completing a full course, you’re not “cured”-you’re just tolerant for now
Where It’s Done
This isn’t something your local pharmacy or general clinic can handle. You need a specialized allergy-immunology center with experience in drug desensitization. Major hospitals like Brigham and Women’s Hospital in Boston have dedicated desensitization units. Their teams have performed thousands of procedures. They have written protocols for over 100 different drugs. They know how to handle reactions, how to adjust for asthma, how to modify for children or elderly patients. In Canada, similar services exist at large academic hospitals-like the Halifax Infirmary, Toronto General, or Montreal’s McGill University Health Centre. But access is limited. If your doctor recommends desensitization, they’ll refer you to an allergist who specializes in this area.
The Big Picture
Drug desensitization has changed the game for people who once had no options. A patient with cystic fibrosis who’s allergic to all available antibiotics? Desensitization lets them breathe easier. A woman with breast cancer allergic to her only effective chemo? She gets to keep fighting. Someone with Crohn’s disease who can’t tolerate their biologic? They get back their quality of life. Studies show success rates above 90% when protocols are followed correctly. The American Academy of Allergy, Asthma & Immunology (AAAAI) updated its guidelines in 2022 to reflect how common and critical this procedure has become-especially with the rise of targeted cancer therapies and biologic drugs. It’s not perfect. It’s not easy. But for many, it’s the only path forward.What to Expect Before, During, and After
Before: You’ll have a detailed consultation. Your allergist will review your reaction history, confirm the allergy with testing if needed, and explain the risks. A written plan will be made for your specific drug and dose schedule. During: You’ll be in a monitored room. Nurses and doctors will watch you closely. You’ll get small doses over hours. You might feel a bit flushed or itchy at first-that’s normal. If you feel anything worse, speak up immediately. After: You’ll be observed for at least an hour after the final dose. If all goes well, you’ll be discharged with instructions to take the drug as prescribed. If you miss a dose, call your team before restarting. Don’t try to pick up where you left off on your own.Questions You Should Ask
- Is there a safe alternative drug I haven’t tried yet?
- What’s the success rate for this specific drug in your center?
- What happens if I react during the procedure?
- How long will the tolerance last if I stop the drug?
- Do you have a written protocol for this exact medication?
- Who will be in the room during the procedure?
Final Thoughts
A drug allergy doesn’t have to be a dead end. With the right team, the right protocol, and the right timing, you can still get the treatment you need. Drug desensitization isn’t magic-but it’s science that works. And for many, it’s the difference between life and loss.Can I try drug desensitization at home?
No. Drug desensitization must be done under direct medical supervision in a hospital or specialized clinic. It requires constant monitoring of vital signs, immediate access to emergency medications like epinephrine, and trained staff who know how to respond to severe reactions. Attempting this at home is extremely dangerous and can be fatal.
How long does a drug desensitization procedure take?
For intravenous drugs like antibiotics or chemotherapy, it typically takes 5 to 6 hours. For oral drugs like aspirin or NSAIDs, it can take several days because doses are spaced further apart. The timeline depends on the drug, your reaction history, and how your body responds during the process.
Is drug desensitization permanent?
No. Desensitization creates only temporary tolerance. If you stop taking the drug for more than 12 to 24 hours, your allergy can return. For chronic conditions, you may need to repeat the process each time you restart the medication. It doesn’t change your immune system permanently-it just lets you tolerate the drug while you’re actively taking it.
What drugs are most commonly desensitized?
The most common include penicillin and other antibiotics, chemotherapy drugs like paclitaxel and carboplatin, biologics such as rituximab and infliximab, aspirin and NSAIDs, and local anesthetics. These are drugs that are either essential for treatment or have no effective alternatives.
Are there any risks of doing drug desensitization?
Yes. There’s always a risk of a severe allergic reaction during the procedure, including anaphylaxis, low blood pressure, or airway swelling. That’s why it’s only done in controlled settings with emergency equipment and trained staff. However, when performed by experienced teams using established protocols, the success rate exceeds 90%.
Can children undergo drug desensitization?
Yes. Children with life-threatening infections or cancer who are allergic to essential medications can be desensitized. Protocols are adjusted for weight and age, and extra care is taken with monitoring. Pediatric allergy centers with experience in this area handle these cases.
What if I have asthma? Can I still be desensitized?
Yes, but extra precautions are taken. Spirometry tests are done before and after each dose to monitor lung function. Dose increases may be slowed, and steroids or bronchodilators may be given ahead of time. Many patients with asthma successfully complete desensitization, especially when their asthma is well-controlled beforehand.
How do I find a center that does drug desensitization?
Ask your doctor to refer you to an allergist-immunologist who specializes in drug hypersensitivity. Major academic medical centers, especially those with allergy clinics or cancer centers, typically offer this service. In Canada, centers in Halifax, Toronto, Montreal, and Vancouver have experience with these procedures. Don’t hesitate to ask if they’ve performed desensitization for your specific drug before.





11 Comments
It’s wild how medicine can bend reality like this. You’re not cured, you’re just given a temporary pass. Like borrowing a life you didn’t earn. Makes you wonder what else we’re temporarily tricking our bodies into accepting.
They say it’s ‘safe’… but have you ever read the fine print on how many people die during desensitization and get quietly buried in the data? Big Pharma loves this. Keeps people dependent. And don’t get me started on the ‘no alternatives’ line-there’s always a cheaper, safer option if you dig deep enough.
Bro this is actual magic 🤯 I know someone who did this for paclitaxel and now she’s back to hiking every weekend. It’s not perfect, but it’s a second chance. I cried watching her get the last dose. No one talks about how emotional this is-like your body finally lets you live again. Also, if you’re scared, just remember: they’re watching you like a hawk. You’re not alone in that room.
.....This is just... a band-aid on a bullet wound. And they charge thousands for it. And you have to sit there for hours, waiting to die. And if you miss a dose? Start over. And what if you’re elderly? Or have asthma? Or... what if they just... mess up? Why isn’t this more regulated? Why aren’t there more lawsuits? Why isn’t anyone talking about the real cost?
One must exercise extreme caution in the application of such a procedure, as the ethical implications of inducing temporary tolerance to a known allergen-without addressing the root immunological dysfunction-are profound. The medical community’s enthusiasm for this intervention appears disproportionate to the long-term risk profile, and the absence of longitudinal data is troubling. One cannot simply substitute expedience for epistemological rigor.
In India we dont have this luxury. My cousin had cancer and allergic to chemo. They gave her alternative drug. She died. No one here has a lab to do this. You guys are lucky. We just pray. And hope. And pay whatever they ask. No one cares if you live or die. This is why I moved to Canada. At least there they try.
I just don’t get why people don’t just avoid the drug entirely. Like… if you’re allergic, why not just find another way? This sounds like a nightmare. I’d rather die than sit there for 6 hours getting tiny doses of poison.
Okay but like… imagine being the nurse who has to do this every day. 😭 I can’t even handle a flu shot. Watching someone go through this… I’d cry every time. Also why is it always ‘oh just go to a big hospital’? What if you live in Nebraska? There’s no center for 500 miles. This system is broken.
This gives me hope. I know someone who was told they’d never get another chemo cycle. They did this. They’re alive. They’re painting again. They’re laughing with their grandkids. It’s not perfect. It’s not easy. But it’s possible. And if you’re scared? That’s okay. Just find a team you trust. You’re not alone. You’ve got this.
In my village we used to treat allergies with turmeric and honey. Now I see this. I think science is amazing. But we must not forget the human side. The fear. The silence in the room. The hand holding. This is not just a protocol. It is a story of courage. And we must tell those stories. Not just the numbers.
I had this done for vancomycin. I screamed the whole time. I thought I was going to die. My mom held my hand. I still have nightmares. But I’m alive. And I hate that this is the only way. And I hate that no one talks about how much it costs. And I hate that my insurance barely covered it. And I hate that I have to do it again next month. I’m tired.