
It’s not just about getting drunk. Mixing alcohol with your prescription meds can turn a routine night into a medical emergency - even if you only have one drink. You might think it’s harmless, especially if your doctor never mentioned it. But the truth is, alcohol and prescription drugs can interact in ways that are silent, deadly, and completely preventable.
How Alcohol Changes How Your Medications Work
Alcohol doesn’t just make you sleepy. It messes with your body’s ability to process medications. There are two main ways this happens: pharmacokinetic and pharmacodynamic interactions.Pharmacokinetic interactions are about absorption and metabolism. Your liver uses enzymes - especially the CYP450 family - to break down both alcohol and most prescription drugs. When you drink, it can either slow down or speed up this process. If alcohol slows it down, your medication builds up in your blood. Too much can lead to overdose. If it speeds it up, your drug gets cleared too fast. That means it stops working - like when someone takes propranolol for high blood pressure and drinks regularly. Their blood pressure spikes because the drug isn’t staying in their system long enough.
Pharmacodynamic interactions are even scarier. This is when alcohol and your medication team up to amplify effects. Think of it like pressing the gas and brake at the same time - your body can’t handle the chaos. Benzodiazepines like Xanax or Valium already slow your brain and breathing. Add alcohol? Sedation jumps by 400%. That’s not just drowsiness. That’s stopped breathing. That’s death.
Medications That Can Kill You With Just One Drink
Not all drugs are created equal when mixed with alcohol. Some are risky. Others are outright dangerous.Opioids - oxycodone, hydrocodone, fentanyl - are the worst offenders. Alcohol and opioids together increase the risk of fatal respiratory depression by six times. In 2022, alcohol-opioid combinations caused 2,318 overdose deaths in the U.S. alone. And it doesn’t take much. A blood alcohol level of just 0.02% - about one standard drink - doubles the chance of a fatal crash when combined with therapeutic opioid doses. Many people don’t realize they’re on opioids until it’s too late. Painkillers after surgery? That’s often where it starts.
Benzodiazepines - used for anxiety, insomnia, seizures - are equally deadly when mixed with alcohol. The American Geriatrics Society calls this combination one of the most preventable causes of death in older adults. Falls, confusion, coma - all become far more likely. In nursing homes, 78% of falls involving sedatives happened when the patient had alcohol within six hours.
NSAIDs like ibuprofen or naproxen seem harmless. But with alcohol? They can cause stomach bleeding. Heavy drinkers (three or more drinks a day) face a 300% higher risk of upper GI bleeding. One study of 200,000 patients showed this wasn’t rare - it was predictable.
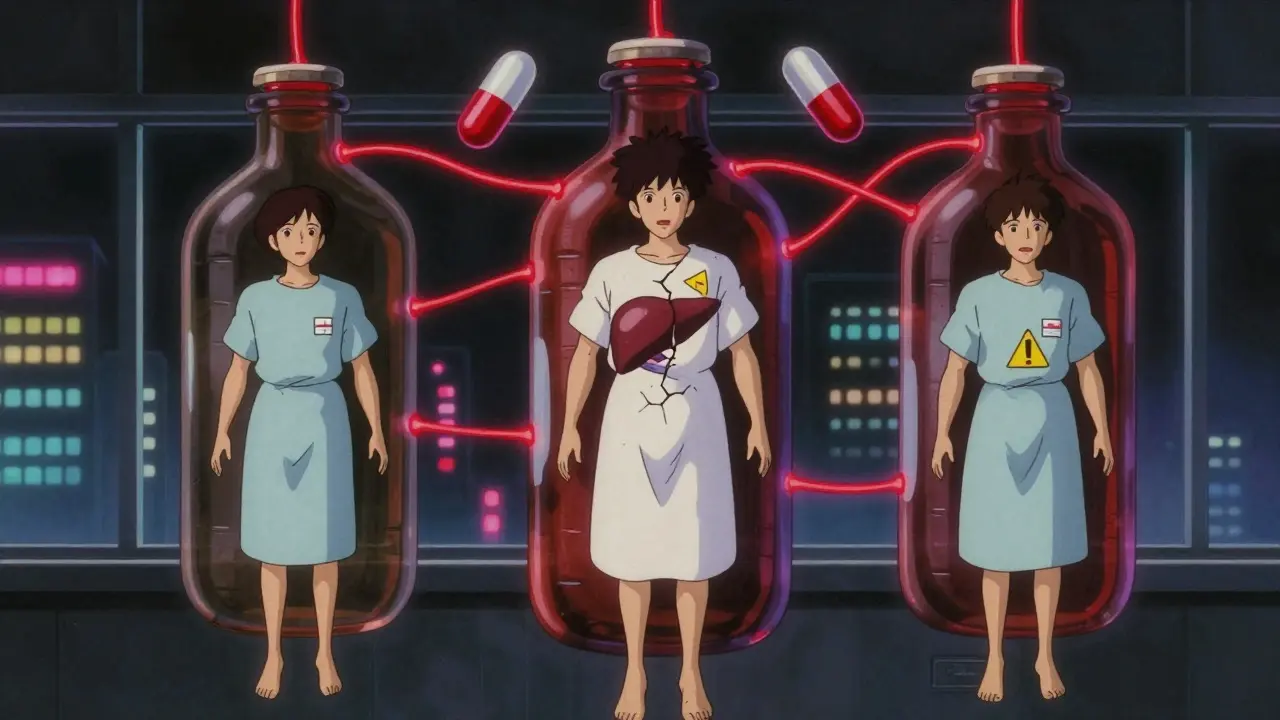
Acetaminophen - Tylenol - is another silent killer. It’s safe when used alone. But with alcohol? It turns toxic. Your liver produces a dangerous byproduct that can cause acute liver failure. One in 200 regular drinkers who take acetaminophen end up in the hospital because of this. The FDA issued a safety alert in 2020. Most people still don’t know.
Who’s at Highest Risk?
This isn’t just about how much you drink. It’s about who you are.If you’re over 65, your body processes alcohol and drugs slower. Your liver isn’t as efficient. Your brain is more sensitive. Adults 65+ have 3.2 times more severe interactions than younger people. And yet, 42% of older U.S. adults are still drinking while taking medications with known interaction risks.
Women are more vulnerable too. Even at the same weight, women have less water in their bodies. That means alcohol stays more concentrated in their blood. They feel the effects faster - and more intensely. A drink that’s fine for a man might be dangerous for a woman on the same medication.
If you have liver disease, your risk skyrockets. Your liver is already damaged. Adding alcohol and acetaminophen? That’s like pouring gasoline on a fire. Your chance of liver failure goes up fivefold.

What You’re Not Being Told
You’d think doctors and pharmacists would warn you. But they often don’t.Healthgrades reviewed 12,450 patient reviews. Of those prescribed benzodiazepines, 68% said their doctor never mentioned alcohol risks. Same with opioids. Patients report being handed prescriptions with no warning - then ending up in the ER after one drink.
Pharmacists are often the last line of defense. One patient in Halifax told their Walgreens pharmacist they drank a glass of wine every night. The pharmacist refused to fill the lorazepam prescription. “Probably saved my life,” the patient wrote. That’s not an outlier. Pharmacies with strong screening protocols reduce interaction-related hospitalizations by 30%.
Even the labels on your meds are unreliable. Only 38% of benzodiazepine prescriptions include a clear alcohol warning. The rest? Silent. You’re expected to know. But most people don’t.
What You Can Do Right Now
You don’t need to be a medical expert to protect yourself. Here’s how:- Check the label. Look for the word “alcohol” or “do not drink.” If it’s not there, assume it’s risky.
- Ask your pharmacist. They’re trained to catch interactions. Ask: “Is it safe to drink while taking this?” Don’t wait for them to ask you.
- Use the NIAAA Alcohol Medication Check app. It’s free. It cross-references over 2,300 medications. Just scan your prescription or type the name.
- Know your risk level. Red = high risk (opioids, benzodiazepines). Yellow = moderate (some blood pressure meds). Green = low (some antibiotics). But green doesn’t mean zero risk.
- Be honest. If you drink - even one drink a week - tell your doctor. They can’t help if they don’t know.
Why ‘Just One’ Isn’t Safe
People say, “I only have one beer with my painkillers.” Or, “I had a glass of wine with my anxiety meds - no problem.” But that’s the trap.One drink can be enough to tip someone over the edge - especially if they’re older, on multiple medications, or have liver issues. The effects aren’t always immediate. Sometimes, they build up over days. You might feel fine today. Tomorrow, you collapse.
A Reddit user from Toronto shared their story: prescribed oxycodone after wisdom teeth surgery. Had two beers. Couldn’t breathe for 20 minutes. Called 911. They survived. But many don’t.
The Bigger Picture
This isn’t just about individual choices. It’s a public health crisis. The global market for drug interaction software is growing fast - hitting $2.8 billion by 2030. Hospitals are using AI to flag risks before a prescription is even filled. The CDC wants to cut overdose deaths by 50% by 2025.But technology won’t fix this alone. People need to know. Doctors need to talk. Pharmacists need to intervene. And patients need to speak up.
If you’re taking a prescription - especially for pain, anxiety, or sleep - don’t assume it’s safe with alcohol. Assume the opposite. Until you’ve confirmed it with a professional, treat it like a loaded gun.
Can I have one drink with my prescription medication?
It depends on the medication. For high-risk drugs like opioids or benzodiazepines, even one drink can be deadly. For others, like some antibiotics, it may be low risk - but never assume. Always check with your pharmacist or doctor. There’s no universal safe amount.
What should I do if I already drank and took my medication?
If you feel dizzy, confused, have trouble breathing, or feel extremely sleepy, call emergency services immediately. Don’t wait. If you’re unsure, call your pharmacist or poison control. They can help you assess your risk based on what you took and how much you drank.
Are over-the-counter meds safe with alcohol?
No. Many OTC drugs carry hidden risks. Acetaminophen (Tylenol), NSAIDs like ibuprofen, and sleep aids like diphenhydramine (Benadryl) can all interact dangerously with alcohol. Always read the label. If alcohol is mentioned, avoid it.
Why don’t doctors always warn patients about alcohol interactions?
Time constraints, assumption that patients know, or lack of training. A 2023 study found 43% of primary care doctors couldn’t correctly identify all high-risk medication classes. Many don’t realize how common and deadly these interactions are. That’s why you need to ask - don’t wait for them to tell you.
Is it safe to drink the day before or after taking medication?
For high-risk drugs like opioids or benzodiazepines, the interaction window can last days. Alcohol stays in your system for hours, but its effect on liver enzymes can linger for days. If you’re on a medication with known interaction risks, avoid alcohol entirely - not just on the day you take it.
What if I’m on multiple medications?
The risk multiplies. Taking three or more medications with alcohol increases the chance of a serious interaction by 70%. Use a medication review tool like the NIAAA app or ask your pharmacist for a full interaction check. Many pharmacies offer free med reviews - take advantage.


8 Comments
Wow. Just... wow. I thought I was being careful having one glass of wine with my Zoloft, but now I'm realizing I might've been playing Russian roulette with my liver. My doctor never said a word. Guess I'm lucky I didn't end up in the ER. Time to call my pharmacist tomorrow.
THIS is why the government doesn’t want you to know. Big Pharma and the FDA are in bed together. They let these deadly combos slide because they make more money off ER visits and lawsuits. Meanwhile, your grandma’s falling down in her nursing home because the label didn’t say ‘DON’T DRINK’ in neon lights. Wake up, people. This isn’t negligence - it’s intentional.
I took ibuprofen with a beer after a long day and felt fine so I thought it was okay. Now I’m reading this and realizing I might’ve been lucky. I’ve been on blood pressure meds for two years and never thought to ask about alcohol. My liver’s probably screaming right now. I’m gonna get a med review next week.
Thank you for sharing this critical information with such clarity and urgency. This is exactly the kind of public health education that saves lives - not just through awareness, but through actionable steps. The NIAAA app alone could prevent thousands of preventable incidents. Please continue to advocate for transparency, accountability, and patient empowerment. Your voice matters.
I’m from the South and we’ve got a lot of folks who take painkillers after surgery and then have a beer or two with dinner. I’ve seen it. I’ve done it. Never thought twice. But now I’m thinking - maybe it’s not just ‘Southern hospitality.’ Maybe it’s just dangerous. I’m gonna tell my cousin who’s on oxycodone after his knee surgery. He needs to hear this from someone he trusts.
So let me get this straight - I can’t have one beer with my Tylenol, but I can down six shots of tequila and still drive? Thanks, America.
Did you know the CIA used to test alcohol-drug combos on soldiers during the Cold War? That’s why they never warn you - they already know how deadly it is and they’re waiting for the right time to use it. Also, your phone is listening when you ask your pharmacist. They’re tracking who’s asking about alcohol and meds. Be careful.
Just read this and immediately texted my mom who’s on Xanax and drinks wine every night 😳 I’m so glad I found this. I’m printing it out and handing it to her with a hug. 🫂