
Why So Many Older Adults Skip Their Medications
Imagine waking up every morning to a table full of pills-ten different colors, shapes, and times to take them. Some need to be taken with food, others on an empty stomach. One makes you dizzy if you stand too fast. Another causes your hands to shake. You’re not sure if the new dizziness is from the medicine or just getting older. You skip a dose because you’re out, or you can’t afford it this month. You don’t tell your doctor because you don’t want to be seen as difficult. This isn’t rare. It’s everyday life for millions of older adults.
Eighty-eight percent of people over 65 take at least one prescription drug. More than half take four or more. That’s not just a number-it’s a daily battle. And when people don’t take their meds as prescribed, the consequences are serious: more hospital visits, worse heart and kidney health, and even early death. The CDC reports that over 200,000 older adults die each year in the U.S. because they didn’t take their medications properly. That’s more than car accidents or falls. Yet, most solutions focus on reminding people to take pills-not fixing the real reasons they stop.
The Real Reasons Older Adults Don’t Take Their Meds
It’s easy to blame forgetfulness. But that’s only part of the story. The biggest barrier isn’t memory-it’s complexity. Taking five or more pills a day, at different times, with different rules, is overwhelming. Studies show that people who take one pill a day are far more likely to stick with it than those juggling three or four doses. When you add in side effects like nausea, dizziness, or confusion, it’s no wonder people start skipping doses-or stop entirely.
Cost is another silent killer. One in three older adults cuts pills in half, delays refills, or skips doses because they can’t afford them. Women, Black, and Hispanic seniors are hit hardest. Food-insecure seniors are six times more likely to skip meds than those who can afford groceries. And here’s the cruel twist: many of these people have insurance. But high deductibles, copays, and tiered pricing still leave them choosing between medicine and meals.
Physical barriers matter too. Arthritis makes it hard to open childproof caps. Poor eyesight makes tiny print on pill bottles unreadable. Weak hands can’t crush pills or use pill organizers. Some seniors can’t even tell if they’ve already taken their morning dose. And then there’s the fear. Many older adults think side effects like falls, memory lapses, or incontinence are just part of aging-not signs their meds are out of balance.
But perhaps the most overlooked issue is isolation. Nearly one-third of adherence problems come from lack of social support. No one to help open bottles. No one to remind them. No one to call the pharmacy when the refill is late. Loneliness doesn’t just hurt emotionally-it hurts physically by making medication management impossible.
What Actually Works: Simple, Proven Fixes
There’s no magic bullet. But there are real, practical steps that work-when they’re done right.
Simplify the regimen. Ask the doctor: Can we cut this down? Are any of these drugs doing the same thing? Can we switch to once-daily versions? Many seniors can cut their pill count in half with smart changes. A 2024 study found that reducing daily doses from three to one boosted adherence by 40% in just six weeks.
Use a pill organizer with alarms. Simple plastic boxes with morning, afternoon, evening, and night compartments help. But better ones come with built-in alarms or phone alerts. Some even connect to apps that notify family members if a dose is missed. These aren’t high-tech gadgets-they’re tools. And they work. One nursing home in Halifax saw a 60% drop in missed doses after introducing automated dispensers.
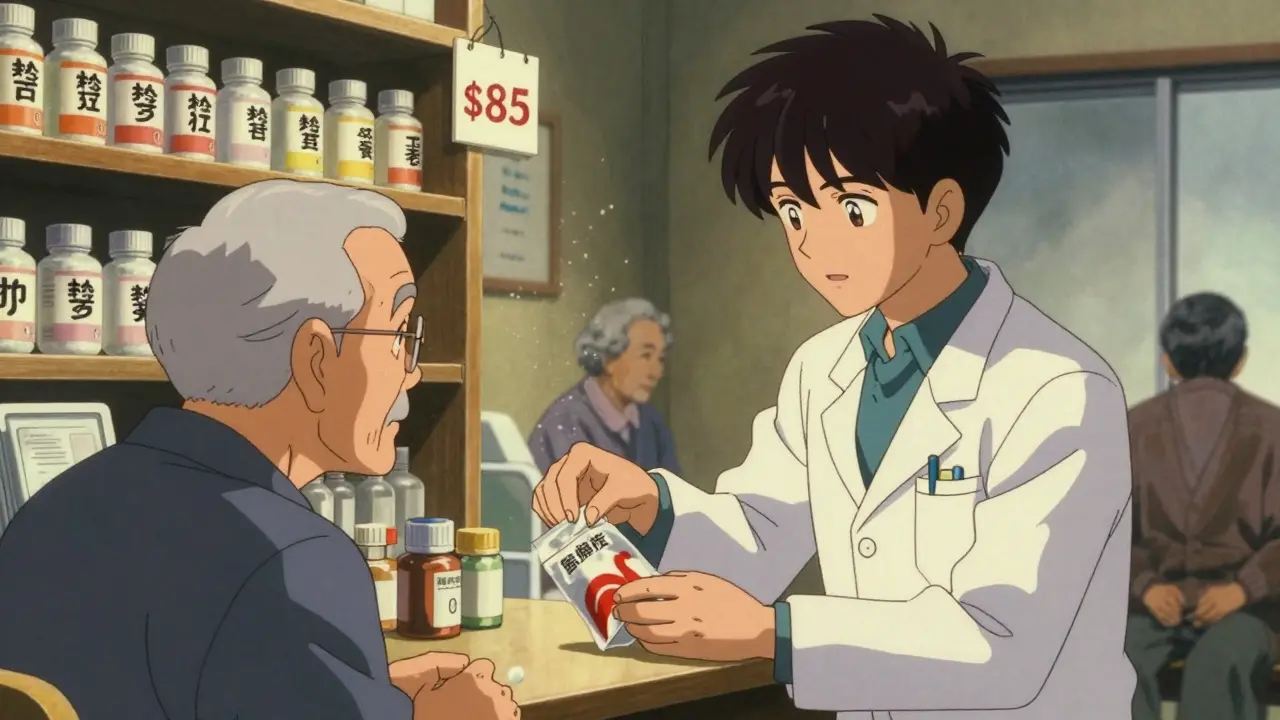
Get help from a pharmacist. Pharmacists aren’t just people who hand out pills. They’re trained to spot drug interactions, unnecessary medications, and cost-saving options. Many offer free med reviews. Ask for one. Bring all your pills-prescription, over-the-counter, vitamins-in a bag. Let them sort it out. A pharmacist might find you’re taking two drugs for the same condition, or that a cheaper generic exists.
Link meds to daily habits. Take your pill after brushing your teeth. After breakfast. After your afternoon tea. Tying medication to a routine you already do makes it automatic. No reminders needed.
Ask for help from family or neighbors. If you live alone, ask a friend, church member, or volunteer to check in once a week. They don’t need to be a nurse-just someone who calls to say, “Did you take your blood pressure pill today?” That small check-in can prevent a crisis.
How to Talk to Your Doctor Without Feeling Guilty
Many seniors don’t tell their doctors they’re skipping meds because they fear being judged. But doctors need to know. Here’s how to bring it up:
- “I’ve been having trouble keeping up with my pills. Can we make this easier?”
- “I’m not taking all of them because they’re too expensive. Is there a cheaper option?”
- “I stopped the heart pill because I felt dizzy. Is that normal?”
Doctors can’t fix what they don’t know. And they’re more likely to help if you’re honest. Many now use “medication reconciliation” during visits-going through every pill you take to cut out the ones that aren’t needed. Don’t wait for them to ask. Bring it up.
What to Do If You Can’t Afford Your Meds
There are options-even if you think you’re stuck.
- Ask your pharmacist about patient assistance programs. Many drug companies give free or low-cost meds to low-income seniors.
- Check if your state has a prescription drug assistance program. In Canada, some provinces offer additional subsidies beyond federal coverage.
- Switch to generic versions. They’re chemically identical but cost 80% less.
- Buy in bulk. Some pharmacies offer 90-day supplies at lower copays.
- Use mail-order pharmacies. They often have lower prices and deliver right to your door.
And if you’re choosing between food and medicine, talk to a social worker. Food banks often have partnerships with clinics to help seniors get their prescriptions.
Technology That Helps-Without Being Complicated
You don’t need a smartphone to use tech that helps. Here are simple tools:
- Pill dispensers with alarms: Devices like MedMinder or Hero send alerts and unlock compartments at the right time. Some even call a family member if a dose is missed.
- Smart pill bottles: Caps like AdhereTech track when the bottle is opened and send a text to a caregiver if it’s been days since the last dose.
- Voice assistants: Say, “Alexa, remind me to take my blood pressure pill at 8 a.m.” It’s that easy.
These tools aren’t for everyone. But if you’re tech-curious, start with one. Many libraries and senior centers offer free demos.

When a Change in Behavior Is a Red Flag
Sometimes, a senior stops taking meds because they feel worse. That’s not laziness-it’s a signal. Dizziness, confusion, falls, or new stomach pain might not be aging. They might be side effects. If someone suddenly stops taking their meds, don’t assume they’re being stubborn. Ask: “Did something happen when you took it?”
Doctors need to know if a medication is causing more harm than good. Sometimes, stopping a drug is the best thing a patient can do. But it should be done with guidance-not in secret.
What Families Can Do
If you’re helping an older parent or relative:
- Don’t assume they’re fine because they say they are.
- Go to one doctor’s appointment with them. Take notes.
- Help them organize their pills once a week. Make it a routine-like Sunday morning coffee.
- Check their medicine cabinet. Are there expired pills? Duplicate prescriptions?
- Ask if they’re skipping doses because of cost. Don’t wait for them to ask for help.
It’s not about control. It’s about safety.
The Bottom Line: Adherence Isn’t About Willpower
Medication adherence isn’t a personal failure. It’s a system failure. Older adults aren’t lazy. They’re overwhelmed. The system asks them to manage complex regimens, pay high prices, and navigate confusing instructions-all while dealing with aging bodies and shrinking support networks.
But change is possible. It starts with asking: What’s really stopping them? Is it the number of pills? The cost? The loneliness? Once you know, you can fix it.
One pill, one reminder, one conversation at a time. That’s how lives get saved-not with grand programs, but with simple, human solutions.





11 Comments
I used to help my grandma with her meds and honestly? The pill organizer with alarms was a game-changer. She’d forget she already took her blood pressure pill and end up doubling up. Now she gets this little box that beeps and lights up. And if she misses it? Her daughter gets a text. Simple. No tech overload. Just human care with a little gadget help.
Also, pharmacists? They’re unsung heroes. My grandma’s pharmacist found she was on two different drugs for the same thing. Cut one. Saved her $120 a month. She cried. Not from sadness-from relief.
I’m a nurse and I see this every single day. It’s not about being forgetful. It’s about being overworked by the system. One woman told me she skips her diabetes med because she’s scared of low blood sugar-and no one ever explained how to handle it. We treat adherence like a discipline problem when it’s actually a communication failure. Talk to them. Not at them. Listen. Then fix.
Y’all are overcomplicating this. It’s called compliance. If you can’t follow a simple regimen, you shouldn’t be on 7 meds. The real issue is lazy doctors prescribing like it’s a buffet. I’ve seen seniors on 11 drugs for conditions that don’t even exist anymore. Deprescribing isn’t a trend-it’s medicine. Stop blaming the elderly. Start blaming the prescribers.
This is the result of losing our values. In my village in India, elders were cared for by family. No pills needed. Now everyone is alone, chasing money, forgetting that life is not about taking more medicine but about living with less desire. The West is sick because the soul is sick. A pill cannot heal loneliness.
While the structural and socio-economic dimensions of medication non-adherence in geriatric populations are indeed multifaceted and require systemic intervention, I must respectfully posit that the ontological burden of pharmacological complexity is often exacerbated by the epistemological disempowerment of the elderly vis-à-vis institutional medical authority. The hermeneutic gap between clinical discourse and lived experience remains unaddressed in most policy frameworks.
I’ve studied this for 18 years. The real problem? Polypharmacy isn’t the issue-it’s the lack of pharmacogenomic screening. You don’t know how someone metabolizes drugs until you test their DNA. That’s why 40% of seniors have adverse reactions. We’re flying blind. And yes, I’ve spoken to the FDA. They’re not listening. 😔
I’ve seen this too many times. My uncle skipped his heart meds because he thought the dizziness was normal. Then he had a stroke. The doctor said he should’ve come in sooner. But he was too ashamed. People don’t skip meds because they’re lazy. They skip because they’re terrified of being called a burden. We need to stop making them feel guilty for surviving
my aunt just started using alexa to remind her and its been life changing. no more confusion. no more stress. just say hey alexa remind me to take my pill and boom. done. why do we make this so hard
You know what’s really happening? Big Pharma doesn’t want you to simplify. They make billions off multiple pills. They push new drugs every year that interact with the old ones. The FDA is in bed with them. And the pharmacies? They profit from refill delays. That’s why they don’t push generics. That’s why they don’t train pharmacists to do med reviews. It’s not about health-it’s about profit. And they’re letting old people die so their stock prices stay up.
I work in a rural clinic in South Africa. Same problem. Old folks skip meds because they walk 10km to get them. Or they sell them to buy food. We started giving them one pill a day, and now we see them smiling again. No fancy gadgets. Just one pill. One less worry. Sometimes the simplest fix is the most radical.
The data clearly demonstrates that adherence metrics are most significantly correlated with cognitive load and pharmacokinetic complexity rather than socioeconomic factors alone. When polypharmacy exceeds five agents, the cognitive burden exceeds working memory thresholds in 78% of geriatric populations, per the 2023 JAMA Geriatrics meta-analysis. Simplification protocols must be standardized under CMS guidelines to achieve therapeutic efficacy.