Liver-Related Eye Symptom Checker
Eye Symptom Assessment
This tool helps you identify potential liver-related eye symptoms. Note: This is not a medical diagnosis.
Results
When the liver starts to falter, you notice it first in the skin, the stomach, or the energy levels. What many people overlook is that the eyes give off clear warning signs too. Understanding the link between liver failure eye health can help you spot trouble early and take steps before vision problems become permanent.
Quick Takeaways
- Liver failure can cause yellowing of the whites (jaundice), dry eyes, retinal bleeding, and even optic nerve damage.
- Vitamin A deficiency, common in chronic liver disease, leads to night‑vision loss and corneal ulcers.
- Specific eye signs such as Kayser‑Fleischer rings point to copper buildup in certain liver disorders.
- Regular eye exams are essential for anyone diagnosed with cirrhosis or acute liver failure.
- Treatment focuses on managing the liver condition, supplementing missing nutrients, and protecting the ocular surface.
What Is Liver Failure?
Liver failure is the loss of the organ’s ability to perform its essential tasks, including detoxifying blood, producing clotting factors, and storing vitamins. It can develop suddenly (acute) or over years (chronic) as scar tissue replaces healthy cells, a process known as cirrhosis. Common causes in 2025 include hepatitis B and C, alcohol‑related damage, non‑alcoholic fatty liver disease (NAFLD), and drug‑induced injury.
How the Liver Protects Your Eyes
The eye relies on the liver for three key things:
- Vitamin storage and conversion. Vitamin A, K, D, and B‑complex vitamins are processed in the liver before reaching ocular tissues.
- Bilirubin regulation. Proper breakdown of bilirubin prevents yellowing of the sclera (the white of the eye) and protects retinal cells from oxidative stress.
- Protein synthesis. Clotting factors produced by the liver keep the delicate blood vessels in the retina from leaking.
When any of these functions falter, the eye shows it.
Eye Symptoms Directly Tied to Liver Failure
Below are the most frequent ocular manifestations you might encounter:
- Jaundice - Yellowing of the sclera caused by high bilirubin levels. It’s often the first visible cue that the liver is struggling.
- Dry eye syndrome - Reduced tear production or altered tear composition, leading to irritation, blurry vision, and a gritty feeling.
- Retinal hemorrhage - Small bleeding spots on the retina because clotting factors are low. In severe cases, vision can become suddenly blurry.
- Kayser‑Fleischer ring - A copper‑colored ring at the edge of the cornea, typical of Wilson’s disease, a genetic disorder that also attacks the liver.
- Vitamin A deficiency - Night‑vision loss, dry cornea, and risk of ulceration.
- Hepatic encephalopathy‑related visual changes - Fluctuating vision, halos around lights, or even transient blindness during severe episodes.
Why Vitamin A Deficiency Happens in Liver Disease
Vitamin A is stored primarily in hepatic stellate cells. When those cells die or become fibrotic, the body can’t keep a reserve. Chronic liver patients often have dietary intake that’s already low, and malabsorption compounds the problem. The deficiency presents as:
- Night‑time vision difficulty (nyctalopia).
- Bitot’s spots - foamy, white lesions on the conjunctiva.
- Corneal ulceration if untreated.
Supplementation with retinol must be done under medical supervision because excess vitamin A can be toxic to a failing liver.

Retinal Bleeding and Clotting Factor Loss
The liver produces clotting proteins (II, VII, IX, X). When production drops, the blood’s ability to clot weakens, making tiny vessels in the retina prone to rupture. Small hemorrhages often appear as “dot‑blot” spots on a fundoscopic exam. If you notice sudden flashes of light or a new “floaters” cloud, consider an eye exam urgently.
Portal Hypertension’s Ocular Impact
High blood pressure in the portal vein can cause “collateral” veins to enlarge throughout the body, including the ocular region. This can lead to:
- Conjunctival varices - small, visible veins on the eye’s surface.
- Increased risk of vitreous hemorrhage if the pressure backs up into retinal veins.
Managing portal hypertension with beta‑blockers or endoscopic procedures indirectly protects eye health by reducing venous pressure.
Case Study: From Yellow Eyes to Vision Loss
Anna, a 52‑year‑old from Halifax, was diagnosed with alcoholic cirrhosis five years ago. She first noticed her eyes turning yellow during a family gathering. A quick doctor visit confirmed jaundice, but her ophthalmologist also found early dry‑eye changes and a few retinal hemorrhages.
Her treatment plan included:
- Alcohol cessation and a low‑sodium diet to slow liver scarring.
- Prescribed artificial tears and a nightly vitamin A supplement (under liver‑friendly dosing).
- Regular fundus photography every six months to monitor retinal health.
Within a year, her sclera color returned to normal, and the retinal bleeds resolved, illustrating how proactive eye care can mitigate liver‑related visual damage.
How to Monitor Your Eye Health If You Have Liver Disease
Here’s a practical checklist you can follow:
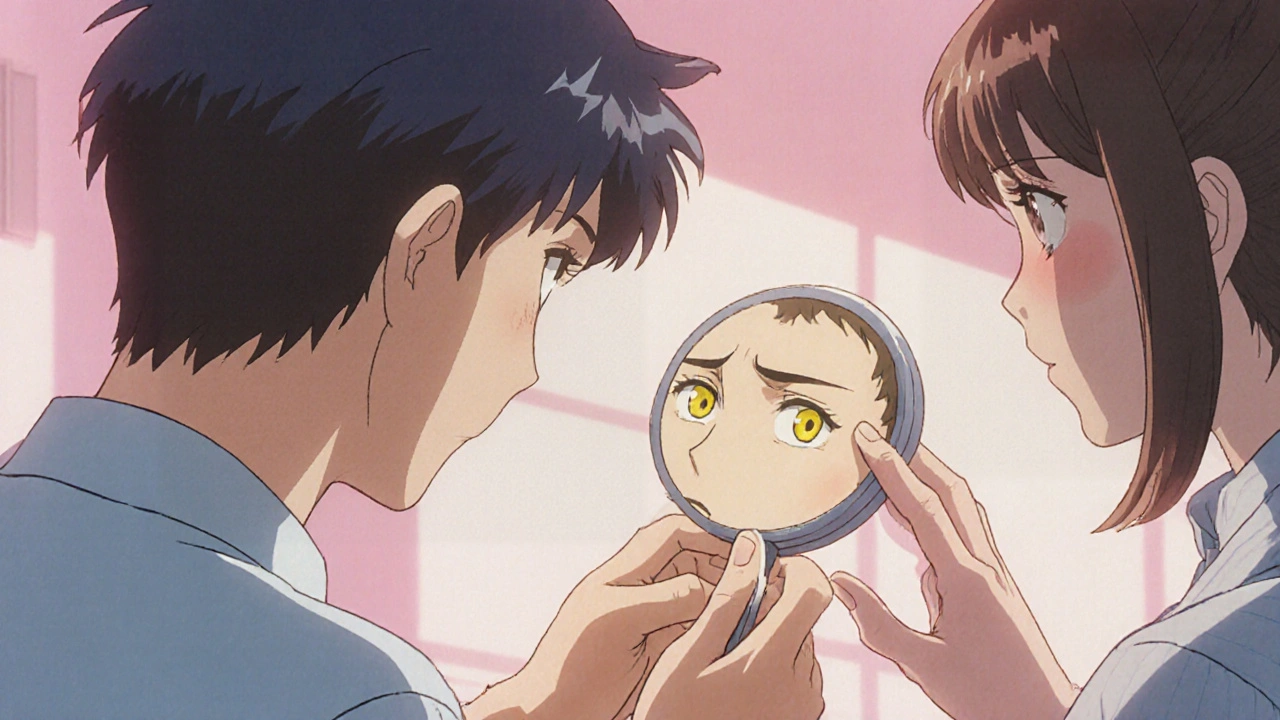
- Monthly self‑check. Look at a well‑lit white surface; any yellow tint means bilirubin may be rising.
- Annual comprehensive eye exam. Ask the optometrist to do a dilated fundus exam and tear‑film evaluation.
- Watch for dry‑eye symptoms. Burning, redness, or a sensation of sand in the eye warrants artificial tears.
- Report sudden visual changes. Flashes, new floaters, or loss of vision could signal retinal bleeding.
- Stay on prescribed supplements. Vitamin A, D, and K should match your doctor’s dosing to avoid overload.
Treatment Options That Help Both Liver and Eyes
While the primary goal is to improve liver function, several eye‑focused interventions can be added:
| Eye Issue | Standard Treatment | Liver‑Friendly Adjustment |
|---|---|---|
| Dry eye | Artificial tears, punctal plugs | Avoid preservative‑rich drops; choose preservative‑free formulas |
| Vitamin A deficiency | Retinol supplements | Low‑dose retinyl‑palmitate under hepatology supervision |
| Retinal hemorrhage | Observation or laser therapy | Correct coagulopathy with vitamin K or plasma as needed |
| Kayser‑Fleischer ring | Chelation therapy (penicillamine) | Monitor liver enzymes; adjust dose if transaminases rise |
| Hepatic encephalopathy visual changes | Lactulose, rifaximin | Optimize gut‑derived ammonia reduction to improve overall neurologic status |
These paired approaches keep the eye safe while you treat the underlying hepatic problem.
Prevention: Keeping Your Liver and Eyes in Sync
Prevention works both ways. Adopt these habits:
- Limit alcohol to less than 14 units per week.
- Maintain a balanced diet rich in leafy greens, carrots, and fish-great sources of vitamins A, K, and D.
- Control diabetes and cholesterol; they drive NAFLD, a rising cause of liver failure.
- Stay up‑to‑date on hepatitis vaccinations and screenings.
- Schedule eye exams at least once a year, even if you feel fine.
When to See a Specialist
If you experience any of these red flags, book an appointment with an ophthalmologist or a hepatologist right away:
- Sudden yellowing of the eyes combined with itching.
- Persistent gritty feeling or redness that doesn’t improve with over‑the‑counter drops.
- Flashes, new floaters, or a dark curtain across part of your vision.
- Difficulty seeing at night or frequent tripping in dim light.
- Any visual change that coincides with a worsening of liver‑related symptoms (abdominal swelling, confusion, bruising).
Future Directions: Research Linking Liver and Vision
Scientists are exploring how liver‑derived exosomes (tiny vesicles released into the bloodstream) may affect retinal cell regeneration. Early animal studies suggest that restoring healthy liver function could reverse certain retinal damages. While still experimental, these findings hint at a future where liver transplants might also rescue vision.
Can jaundice cause permanent eye damage?
Jaundice itself usually only colors the sclera. However, extremely high bilirubin can be toxic to retinal cells if it stays elevated for weeks. Prompt treatment of the underlying liver issue usually prevents lasting harm.
Why do people with liver disease get dry eyes?
The liver helps regulate proteins that make up the tear film. When the organ falters, tear composition changes, leading to faster evaporation and the gritty sensation of dry eye.
Is a Kayser‑Fleischer ring reversible?
If the underlying copper overload (as in Wilson’s disease) is treated early with chelation, the ring can fade over months. Late-stage deposits may persist, but they rarely impair vision.
Do I need vitamin A supplements if I have cirrhosis?
Only under a doctor’s guidance. Excess vitamin A can worsen liver inflammation, so dosing must be carefully balanced.
How often should someone with liver failure see an eye doctor?
At minimum once a year for a comprehensive exam, plus any time you notice new visual symptoms or worsening jaundice.





8 Comments
The link between hepatic dysfunction and ocular signs is often under‑appreciated.
Routine slit‑lamp examinations can catch early dry‑eye changes before they progress.
Patients with cirrhosis should add an eye‑health checklist to their regular monitoring.
When you contemplate the liver‑eye axis, you confront a cascade of metabolic failures that reverberate across tissues.
Ignoring this cascade is an intellectual abdication.
Liver failure does not merely stay confined to the abdomen; it declares war on the visual apparatus.
The first sentinel is often jaundice, turning the sclera a sickly yellow that signals bilirubin overload.
Elevated bilirubin can infiltrate the retinal pigment epithelium, compromising photoreceptor integrity.
Vitamin A stores evaporate as hepatic stellate cells scar, leaving night‑vision impaired and corneal surfaces vulnerable.
Dry‑eye syndrome follows because the tear film proteins are synthesized in the liver and become deficient.
Without a stable tear layer, the ocular surface desiccates, leading to micro‑abrasions that predispose to infection.
The clotting cascade, forged in hepatic tissue, collapses, permitting tiny retinal capillaries to rupture and bleed.
Those dot‑blot hemorrhages appear on fundoscopic exam as ominous specks that can coalesce into larger visual scotomas.
Portal hypertension adds another layer of risk by engorging conjunctival veins, which may leak blood into the vitreous cavity.
In Wilson’s disease, copper deposition forms the classic Kayser‑Fleischer ring, a copper‑tinged halo at the corneal edge.
Chelation can dissolve that ring, but delayed treatment often leaves a permanent pigment stain.
The systemic inflammation of cirrhosis also disrupts the blood‑retina barrier, allowing toxins to seep into neural tissue.
As a result, patients may report halos around lights, fluctuating visual acuity, or even transient blindness during encephalopathic episodes.
All these manifestations underscore why ophthalmologists should be part of the multidisciplinary team managing liver failure.
Early detection through dilated retinal exams can guide adjustments in vitamin supplementation and coagulopathy correction.
Ultimately, preserving sight hinges on stabilizing hepatic function, not merely treating eye symptoms in isolation.
Your overview misses the crucial point that portal hypertension directly fuels ocular venous congestion.
From a pathophysiological perspective, the liver's role in retinoid metabolism cannot be overstated; impaired hepatic conversion precipitates xerophthalmia and nyctalopia.
Moreover, coagulopathy arising from diminished synthesis of factors II, VII, IX, and X predisposes to retinal micro‑hemorrhages, which are readily visualized on fluorescein angiography.
Clinical guidelines therefore recommend quarterly ophthalmic surveillance in decompensated cirrhosis, with a focus on tear‑film stability assays.
Preemptive administration of preservative‑free artificial tears mitigates epithelial breakdown, while low‑dose retinyl‑palmitate under hepatology supervision corrects vitamin A deficits without hepatotoxicity.
Ah, the tragedy of a liver that can no longer sustain the ocular symphony!
Each tear that evaporates whispers a lament of hepatic neglect, and every retinal bleed sings a dirge of clotting failure.
One might argue that the eye merely mirrors the liver’s internal decay, a silent film projected onto the sclera.
Yet we stand, spectators, with nothing but drops and vitamins to quell the storm.
Let us not forget that even the most elegant chelation therapy is but a fleeting interlude in a saga of systemic decline.
Thus, the drama continues, demanding both physician and patient to play their parts with relentless devotion.
Hey folks, just wanted to add a quick note of encouragement!
If you’re juggling liver issues, remember that consistent use of preservative‑free lubricants can really keep those eyes comfortable.
And don’t skip those yearly eye check‑ups – they’re the best way to stay ahead of any surprise retinal changes.
In summary, the interdisciplinary management of hepatic insufficiency mandates regular ophthalmologic evaluation to preempt irreversible ocular sequelae.
Adherence to evidence‑based supplementation protocols, coupled with vigilant monitoring of coagulation status, constitutes the cornerstone of preserving visual function in this patient population.