When a patient picks up a generic pill, they don’t just see a cheaper version of their brand-name drug. They see a color, a shape, a size-and sometimes, a cultural message they didn’t ask for. In Halifax, Toronto, or Los Angeles, a Muslim patient might refuse a capsule because it contains gelatin from pork. A Haitian grandmother might distrust a white tablet because, in her community, only red pills heal high blood pressure. A Latino man might skip his diabetes meds because the generic looks nothing like the brand he remembers from back home. These aren’t just quirks. They’re barriers to health-and they’re happening every day because the system still treats generics as one-size-fits-all.
Generics Aren’t Just Chemicals-They’re Cultural Objects
Generic drugs contain the same active ingredient as brand-name drugs. That’s the science. But the rest? The coating, the dye, the gelatin shell, the imprint on the tablet-that’s where culture steps in. For many patients, these details aren’t random. They carry meaning.
Take gelatin. It’s a common capsule filler. But for Muslims, Jews, and some Hindus, gelatin derived from pork is strictly forbidden. A 2023 study found that 63% of pharmacists in urban clinics get at least one question per week about whether a medication contains animal products. And when the answer is yes? Many patients walk away. Not because they don’t want to get better. Because they can’t in good conscience take it.
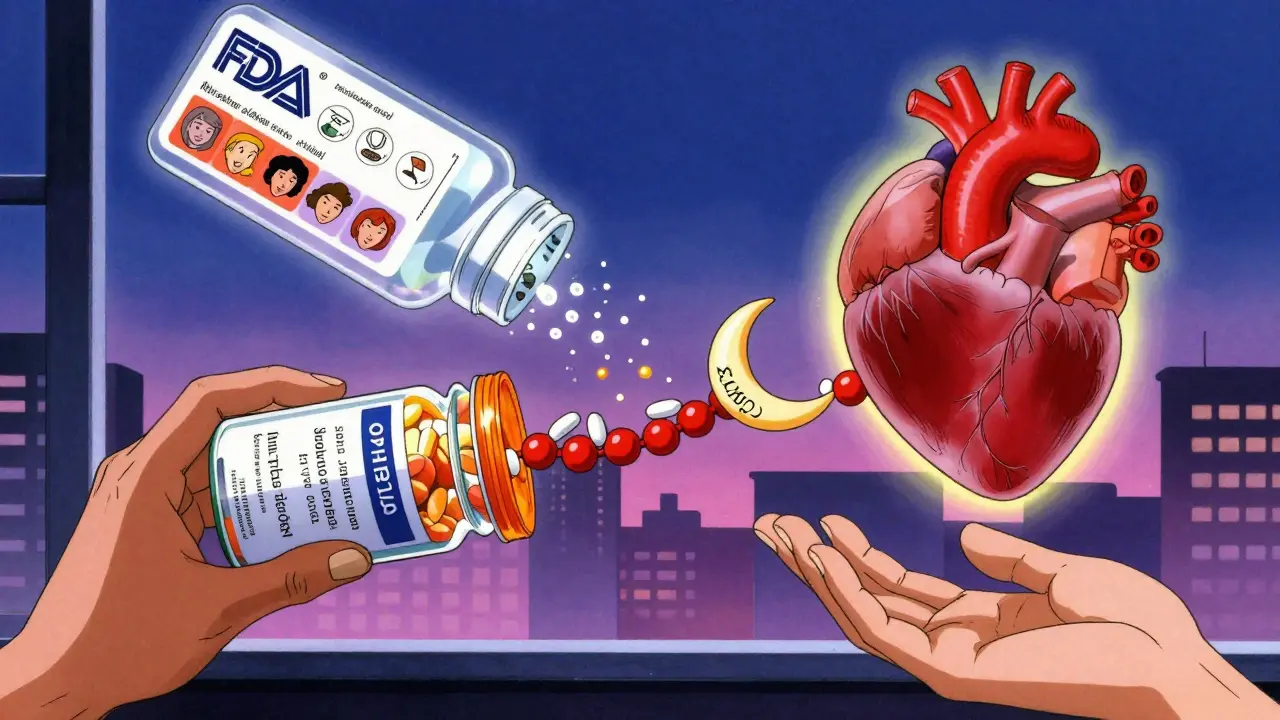
Color matters too. In some Asian cultures, white pills are associated with death or mourning. In parts of Latin America, blue pills are seen as calming, while green ones signal poison. African American patients are nearly twice as likely as white patients to believe generics are less effective-partly because they look different. A 2022 FDA survey showed 28% of African American patients doubted generic effectiveness, compared to just 15% of non-Hispanic white patients. That gap isn’t about science. It’s about history, trust, and lived experience.
Why the System Keeps Failing
The pharmaceutical industry knows this. But fixing it isn’t easy. Generic manufacturers are under pressure to cut costs. Adding halal-certified capsules or kosher-approved dyes means extra steps, extra testing, extra paperwork. And right now, only 37% of generic drug labels in the U.S. even list all the inactive ingredients. In the EU, it’s 68%. That’s a gap. A dangerous one.
Pharmacists are stuck in the middle. One pharmacist in the same 2023 study spent two full hours calling manufacturers just to find a liquid version of a medication without gelatin. Another had to switch a patient from a capsule to a tablet because the patient’s religious leader said the capsule shell was haram. These aren’t edge cases. They’re daily realities in diverse cities.
And the regulatory system? It’s slow. The Food and Drug Omnibus Reform Act (FDORA) passed in December 2022 pushed for better inclusion of diverse populations in clinical trials and recognized social determinants of health. But it didn’t require manufacturers to label excipients clearly. It didn’t mandate culturally adapted packaging. It didn’t fund training for pharmacists on religious dietary laws. So progress is patchy.
What Works: Real Solutions in Real Clinics
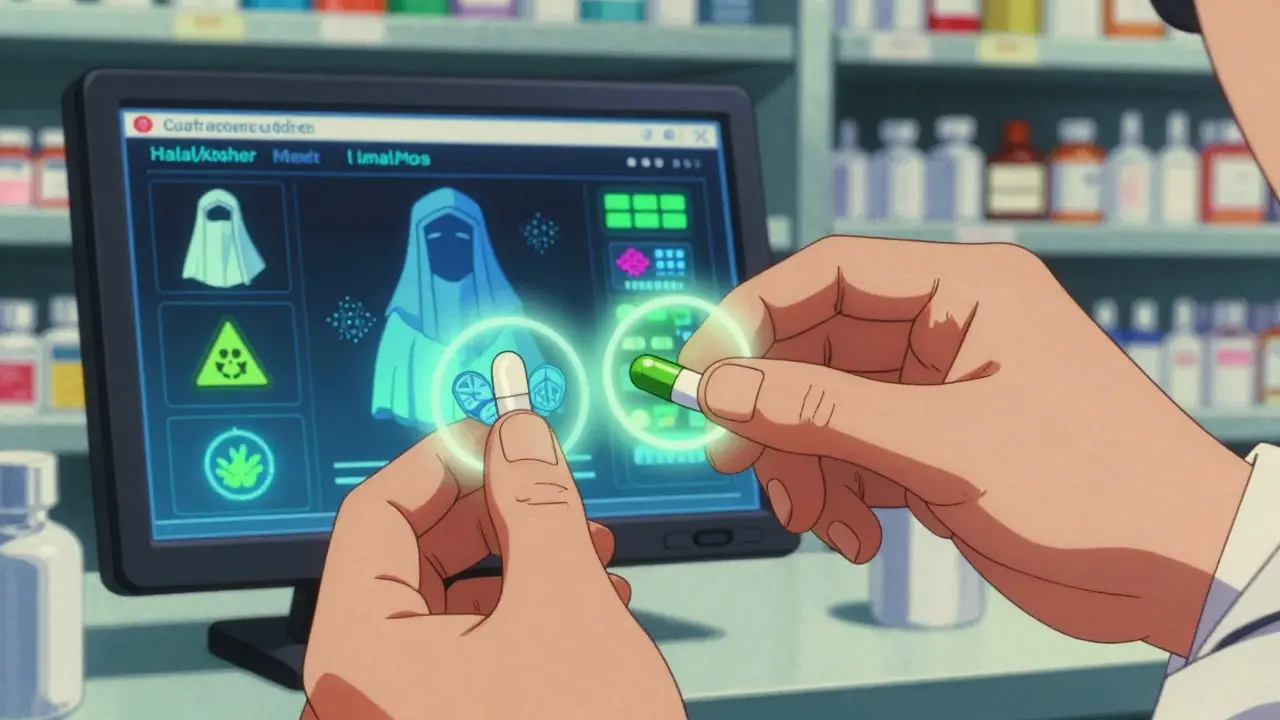
Some places are getting it right. A chain of community pharmacies in Ontario started keeping a digital database of generic medications with halal and kosher certifications. Staff can search by drug name and instantly see which versions are acceptable. Time saved? From hours to seconds.
Another clinic in Toronto trains all new pharmacy techs in cultural competency-covering everything from Islamic dietary rules to how to explain generic substitution to a patient who’s never trusted the healthcare system. They use simple visual aids: a chart showing pill colors and what they mean in different cultures. No jargon. No assumptions.
At the corporate level, Teva Pharmaceutical launched its Cultural Formulation Initiative in 2023. By late 2024, they plan to document excipient sources for all 15 major therapeutic areas. Sandoz is building a Global Cultural Competence Framework. These aren’t PR moves. They’re survival strategies. The global generic market is worth over $500 billion. And 40% of U.S. consumers now identify as non-white. Ignoring cultural needs isn’t just unethical-it’s bad business.
The Hidden Cost of Ignoring Culture
When patients don’t take their meds because of cultural mismatch, the cost isn’t just personal. It’s systemic. Non-adherence to hypertension and diabetes meds alone costs the U.S. healthcare system over $100 billion a year. And minority populations bear the brunt. African Americans are 60% more likely to die from hypertension than white Americans. Latinos have higher rates of uncontrolled diabetes. Many of these outcomes are tied to medication non-adherence.
And it’s not just about religion or color. Language plays a role too. A Spanish-speaking patient might get a generic prescription with English-only instructions. They don’t understand the dosage. They skip a day. Then another. Their blood sugar spikes. They end up in the ER. All because the system didn’t offer instructions in their language-or didn’t bother to check if they understood.
Even the shape of a pill matters. In some cultures, round pills are seen as more natural. Oval ones feel industrial. If a generic changes shape from the brand version, patients assume the drug is weaker-even if it’s chemically identical. That’s perception. But perception drives behavior. And behavior drives outcomes.
What Needs to Change
Here’s what’s needed-and it’s not complicated:
- Clear labeling of all excipients-on every generic package. No exceptions. If it’s pork, soy, or alcohol-based, say it. In multiple languages.
- Training for pharmacy staff-8 to 12 hours a year on cultural beliefs around medicine. Not a one-time seminar. Ongoing.
- Database access-pharmacies need real-time tools to check which generics meet halal, kosher, vegan, or cultural standards.
- More generic options-manufacturers need to produce multiple versions of high-demand drugs with different colors, shapes, and fillers.
- Community partnerships-work with religious leaders, cultural centers, and patient advocates to co-design patient education materials.
This isn’t about making generics more expensive. It’s about making them more usable. And usable means trusted. Trusted means taken. Taken means healthier people.
It’s Not Just About Drugs-It’s About Respect
At its core, this isn’t a technical problem. It’s a human one. A patient doesn’t want to be a statistic. They want to be heard. They want their beliefs honored. They want to know that their faith, their culture, their history matters-even when they’re picking up a $5 pill.
When a pharmacist takes a moment to say, “I know this looks different, but let me show you why it’s the same medicine-and here’s a version that fits your needs,” that’s not just good service. That’s healing.
Generics were meant to make healthcare affordable. But affordability means nothing if the patient won’t take it. Culture isn’t a footnote in pharmacology. It’s the foundation of adherence. And until the system treats it that way, millions will keep walking away from the medicine they need.
Why do some patients refuse generic medications based on color or shape?
Many cultures associate certain colors or shapes with specific meanings-like white for mourning in parts of Asia, or round pills being seen as more natural. When a generic looks different from the brand version, patients may believe it’s weaker, fake, or even dangerous-even if the active ingredient is identical. These beliefs are shaped by cultural norms, not science, and ignoring them leads to non-adherence.
Are there generic medications that meet halal or kosher standards?
Yes, but they’re hard to find. Some manufacturers produce gelatin-free capsules or use plant-based alternatives. Others use bovine gelatin from animals slaughtered according to halal or kosher laws. But this information isn’t always listed on labels. Pharmacists often have to contact manufacturers directly, which can take hours. A few pharmacy chains now maintain searchable databases to speed this up.
How do language barriers affect generic medication use?
Patients who don’t read English may not understand dosage instructions on generic labels. This leads to missed doses, overdoses, or stopping the medication altogether. Simple fixes-like printed instructions in Spanish, Mandarin, or Punjabi-can dramatically improve adherence. Some clinics now use QR codes that link to audio instructions in multiple languages.
Why are African American and Hispanic patients more likely to distrust generics?
Historical discrimination in healthcare, combined with systemic gaps in access and communication, has eroded trust. Many patients from these communities have seen medications fail or been told their symptoms weren’t taken seriously. When a generic looks cheaper or different, it reinforces the belief that they’re getting second-rate care. Addressing this requires not just better labeling, but building long-term trust through consistent, respectful care.
What can pharmacists do today to improve cultural competence?
Start by asking: "Do you have any religious or cultural beliefs about how you take your medicine?" Don’t assume. Keep a list of common excipient concerns (gelatin, alcohol, dyes) and know where to find alternatives. Use visual aids to explain why generics are safe. Partner with local cultural groups to create translated materials. Small steps make a big difference.
Is there a push to make cultural considerations mandatory in generic drug labeling?
Not yet in the U.S., but pressure is growing. The FDA has acknowledged the issue, and the 2022 FDORA law highlighted the need for inclusive care. Companies like Teva and Sandoz are voluntarily improving labeling. But without federal rules, progress remains uneven. Advocacy groups are pushing for standardized excipient disclosure across all generic drugs, regardless of country of origin.
What’s Next for Patient-Centered Generics
By 2027, industry analysts predict 65% of top generic manufacturers will include cultural considerations in their product design. That’s up from just 15% in 2023. The shift isn’t coming because it’s trendy. It’s coming because patients are demanding it-and because the cost of ignoring them is too high.
The future of generics isn’t just about price. It’s about dignity. About respect. About making sure that no matter who you are, where you’re from, or what you believe, the medicine you need doesn’t ask you to choose between your health and your values.





14 Comments
Man, this post hit me right in the feels. I never thought about how a pill’s color could make someone feel like they’re being asked to betray their faith or culture. It’s wild that we still treat medicine like a vending machine-pop in cash, get your dose, no questions asked. But humans aren’t machines. We carry histories in our bones, and if your grandma swore by red pills for blood pressure, seeing a white one feels like a slap in the face. We need to stop treating cultural sensitivity like a bonus feature and start treating it like basic human decency.
In India, we have this thing called ‘pati’-the outer shell of medicine. Many elders believe if it’s not red or yellow, it’s not strong. I’ve seen my aunt refuse insulin because the pill was blue. She said it looked like poison from a TV show. No one laughed. We just found her a yellow version. Culture isn’t irrational-it’s just not coded into the system. Pharma needs to stop thinking in dollars and start thinking in stories.
Let’s be real-this isn’t about culture. It’s about ignorance. People refuse meds because they’re lazy or superstitious. If you can’t follow basic science, don’t blame the pill. The FDA approves these drugs. The chemistry is identical. If you want to believe a white tablet is ‘weaker’ because it doesn’t look like the one from your cousin’s village, that’s not a cultural issue-it’s a cognitive bias. Stop romanticizing noncompliance.
It’s fascinating how deeply embedded symbolic meaning is in pharmaceuticals-how a gelatin capsule isn’t just a delivery mechanism but a theological boundary, how a color becomes a cultural semaphore. We’ve reduced medicine to molecules and dosage, but we’ve forgotten that healing is not just biological-it’s semiotic. The pill is a signifier. It carries the weight of ancestral memory, religious law, and collective trauma. And when the system ignores that, it doesn’t just fail pharmacologically-it fails spiritually. We need a new pharmacopeia-not just of chemicals, but of meaning.
My mom takes blood pressure meds. She won’t take anything that’s not round. Says oval ones feel ‘too corporate.’ I didn’t think much of it until I read this. Now I’m wondering how many people are skipping meds because the shape feels ‘wrong.’ It’s not about logic. It’s about comfort. Maybe we need pill shapes that feel familiar, not just cheap.
Let’s not kid ourselves-this is just woke capitalism in disguise. 🤡 Pharma isn’t doing this out of altruism. They’re responding to demographic shifts and regulatory FUD. The real solution? Educate patients. Stop pandering to superstition. If someone believes a blue pill is poison, they need a therapist, not a new capsule formulation. Cultural sensitivity ≠ medical capitulation.
I work in a pharmacy in Melbourne and we’ve been keeping a little binder of which generics have halal and kosher options. It’s not perfect but it’s saved so many patients from having to call manufacturers. The real win? When a guy came in looking for his diabetes med and said ‘I just need the one that looks like back home’-we had it. He cried. That’s the moment you realize this isn’t about pills. It’s about dignity
I think we’re missing the bigger picture here. This isn’t just about gelatin or color. It’s about trust. So many communities have been burned by the medical system-experimentation, dismissal, neglect. When a generic looks different, it’s not just about the pill. It’s a reminder that they’re still treated as afterthoughts. Fixing the labels won’t fix that. But listening? That might.
Oh here we go. Another ‘culture is king’ lecture. Let me guess-next they’ll say we need different pill shapes for people who believe in astrology. People don’t need more options. They need to stop being lazy and trust science. If your grandmother thinks red pills work better, that’s not a cultural insight. That’s a superstition dressed up as identity. And we’re letting it derail public health.
My cousin is a pharmacist in Chicago. She started asking every patient: ‘Do you have any beliefs about how your medicine should look or feel?’ No jargon. No assumptions. Just a quiet question. And you know what? People opened up. One woman told her she’d been skipping her antidepressants because the capsule was too big-it reminded her of the pills her abusive uncle forced her to take. That’s the real cost of one-size-fits-all. It doesn’t just miss the mark. It retraumatizes.
Look, I get it. But we’re not in the 1800s. We’re in America. If you can’t handle a white pill because your culture says it’s bad, maybe you need to assimilate a little. We don’t make special gluten-free versions of every drug for every dietary whim. This is just another demand for special treatment. The system works fine for most people. Stop making it harder for everyone else.
As someone from India, I’ve seen this firsthand. My grandfather refused a generic because the imprint was ‘M’ instead of ‘C’-he thought ‘M’ meant ‘medicine for the rich’ and ‘C’ meant ‘common.’ We spent weeks finding the exact same drug with a ‘C’ imprint. It’s absurd-but it’s real. The solution isn’t to change culture. It’s to change the system to meet culture halfway.
My dad’s from Guatemala. He still takes his blood pressure meds the way his uncle did in the 70s-red pill, morning, with coffee. When he got a generic that was white, he threw it out. We found a red version. He’s been stable since. It’s not about science. It’s about ritual. And rituals matter.
Just had a patient yesterday ask if the generic was ‘the same as the one from Mexico.’ We didn’t have it. She left. I felt awful. This isn’t about convenience. It’s about continuity. When you’re far from home, the pill is the last thing that feels familiar. We owe them that.