
Diabetes Medication Sugar Impact Calculator
Calculate Your Daily Added Sugar Intake
The American Diabetes Association recommends limiting added sugar to no more than 25 grams per day for optimal medication effectiveness.
Tips for Better Medication Results
Try swapping one sugary item for a healthier alternative:
- Replace soda with water or unsweetened tea
- Choose plain Greek yogurt with cinnamon instead of flavored varieties
- Pair fruits with nuts or seeds to slow sugar absorption
Why This Matters
Research shows: • People who consume over 100g of added sugar daily need nearly 30% more metformin to reach the same blood sugar levels • High-sugar meals can reduce metformin absorption by up to 30% • Consistent carbohydrate intake reduces hypoglycemia episodes by 75%
Key takeaway: Diabetes medications work best when your diet supports them—not fights them. Tracking your sugar intake helps you optimize your treatment and avoid unnecessary complications.
Why Sugar Matters More Than You Think With Diabetes Medications
Take metformin every day. Check your blood sugar. Follow your doctor’s advice. But if you’re still struggling to get your numbers down, the problem might not be the medicine-it’s what you’re eating with it.
Diabetes medications don’t work in a vacuum. They’re designed to help your body manage blood sugar, but they can’t fight off a constant flood of sugar from your plate or your drink. The truth is, no pill, injection, or pump can fully compensate for a diet loaded with added sugars. And that’s not just a suggestion-it’s backed by years of clinical data.
How Metformin Really Works (And Why Sugar Ruins Its Job)
Metformin is the most common first-line drug for Type 2 diabetes. It doesn’t force your body to make more insulin. Instead, it tells your liver to stop dumping out extra glucose and helps your muscles use insulin better. Simple, right?
But here’s the catch: if you eat a bowl of sugary cereal, a soda, and a pastry for breakfast, your body gets hit with over 100 grams of glucose in under 30 minutes. Metformin can only do so much. A 2022 GoodRx analysis found that people who ate more than 100 grams of added sugar daily needed nearly 30% more metformin just to reach the same blood sugar levels as those who kept added sugar under 25 grams.
That’s not a coincidence. High-sugar meals delay how fast metformin gets absorbed. A 2019 study showed peak drug levels dropped by up to 30% after a high-fat, high-sugar meal. That means less of the medicine is working when you need it most-right after eating.
The Hidden Danger: Sugar and Hypoglycemia
If you’re on sulfonylureas like glyburide or meglitinides like repaglinide, sugar isn’t just a problem for high blood sugar-it’s a trigger for low blood sugar.
These drugs force your pancreas to pump out insulin, no matter what. If you eat a big slice of cake, your insulin spikes and your blood sugar drops fast. But if you skip a meal or eat less sugar than usual? Your body still gets the same insulin dose. That’s when your blood sugar crashes.
Cleveland Clinic data shows patients on these drugs who eat inconsistent amounts of carbs have 3 to 5 hypoglycemic episodes per year. Those who eat the same amount of carbs at every meal? Just 1 or 2. That’s a 75% drop in dangerous low-blood-sugar events.
It’s not about cutting sugar entirely. It’s about consistency. Eat 45 grams of carbs at breakfast every day? Your medication can adjust. Eat 15 grams one day and 90 the next? You’re playing Russian roulette with your blood sugar.
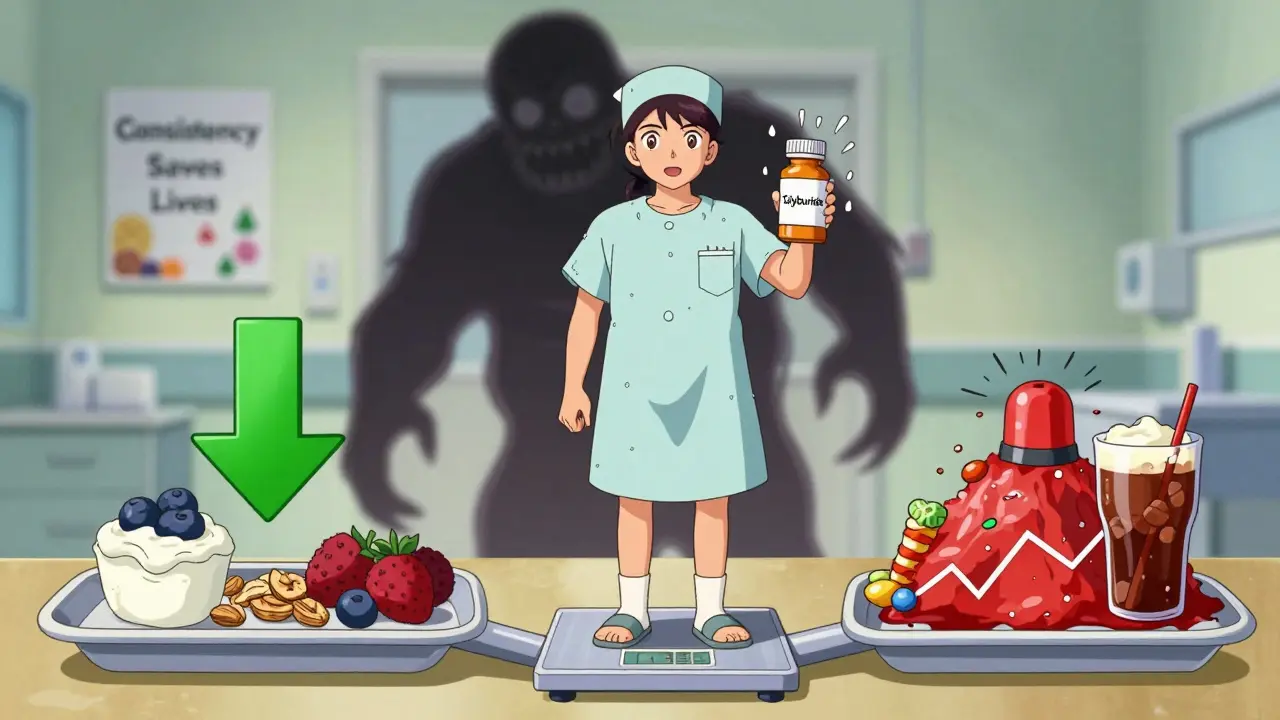
What Foods to Avoid (And What to Choose Instead)
Not all sugar is the same. But when you’re on diabetes meds, you need to treat all added sugar like a red flag.
- Sugary drinks-soda, sweetened tea, fruit juice with added sugar. One 12-ounce soda has 39 grams of sugar. That’s nearly the entire daily limit for added sugar.
- Processed snacks-granola bars, flavored yogurts, packaged cookies. Many have 15-25 grams of sugar per serving, often hidden under names like “cane syrup” or “fruit concentrate.”
- White bread, pastries, and pasta-they break down into glucose faster than table sugar. A single slice of white bread can spike blood sugar more than a candy bar.
- High-sugar fruits-mangoes, grapes, cherries. These aren’t bad, but they’re high in natural sugars. Eat them in small portions with protein or fat to slow absorption.
- Alcohol with mixers-sweet cocktails, rum and coke, wine spritzers. They spike sugar and can mask hypoglycemia symptoms.
Swap them for:
- Whole fruits like berries, apples, and pears (lower sugar, high fiber)
- Plain Greek yogurt with a sprinkle of cinnamon
- Whole grains like oats, quinoa, and brown rice
- Vegetables, legumes, nuts, seeds, and lean proteins
And here’s a game-changer: choose low-glycemic-index (GI) foods. These are foods that release sugar slowly into your bloodstream. Think lentils, chickpeas, non-starchy veggies, and most whole fruits. A 2025 review found that switching to low-GI foods improved insulin sensitivity by 25-40% and cut post-meal blood sugar spikes by 35-50 mg/dL.
Newer Medications Aren’t a Free Pass
You might hear that newer drugs like semaglutide (Ozempic) or dapagliflozin (Farxiga) let you eat whatever you want. They don’t.
These drugs work differently. GLP-1 agonists slow digestion and reduce appetite. SGLT2 inhibitors make your kidneys flush out extra sugar through urine. That sounds like magic, right?
But even these drugs lose effectiveness when sugar intake is too high. A 2023 ADA position statement found that patients on these newer agents who ate more than 100 grams of added sugar daily saw their medication’s effect drop by 15-20%. That’s not nothing. It means you’re still getting the same side effects, but less benefit.
And here’s the kicker: people on these drugs often feel less hungry, so they eat less. That’s great-but if they start eating more sugar because they think the drug will “cover it,” they end up gaining weight, not losing it.
What About Other Medications You’re Taking?
Diabetes doesn’t live in isolation. Many people take other drugs that can make sugar control harder.
Take steroids like prednisone. Just one dose can spike blood sugar by 50-100 mg/dL. If you’re on metformin and get a steroid shot for inflammation? You’ll need tighter sugar monitoring and possibly a temporary med adjustment.
Diuretics like furosemide (Lasix) can make metformin less effective in about one-third of patients. Birth control pills alter how your body handles glucose in nearly 1 in 4 women.
And if you have kidney issues? High sugar + metformin raises your risk of lactic acidosis-a rare but dangerous buildup of acid in the blood. The NHS warns this risk triples in patients with low kidney function (eGFR below 45) who eat a high-sugar diet.
The Real Secret: Medical Nutrition Therapy
Here’s the most overlooked part of diabetes care: talking to a registered dietitian.
A 2024 study found that people who got personalized nutrition counseling when they started their meds reached their target HbA1c in 6.2 months. Those who didn’t? It took nearly 12 months. That’s almost half the time.
And the results go beyond numbers. Patients who worked with a dietitian had 63% fewer emergency visits for blood sugar crashes or spikes. They needed fewer med changes. They felt more in control.
Yet, only 39% of doctors refer new Type 2 patients to dietitians. The American Diabetes Association says everyone should get this support within 30 days of diagnosis. Only 42% of clinics actually do it.
If your doctor hasn’t mentioned a dietitian, ask. If they say, “Just cut the sugar,” push back. That’s not a plan. It’s a suggestion.
What You Can Do Today
You don’t need to overhaul your life overnight. Start small.
- Track your sugar for 3 days. Use a free app or just write it down. Look for patterns. Do you crash after lunch? Do you reach for soda when you’re tired?
- Swap one sugary drink a day for water, unsweetened tea, or sparkling water with lemon.
- Check labels. If sugar is in the top 3 ingredients, reconsider.
- Pair carbs with protein or fat. Eat an apple with peanut butter. Have oatmeal with eggs. It slows the sugar rush.
- Ask your doctor for a referral to a registered dietitian. Don’t wait.
Bottom Line: Medication Isn’t a License to Eat Sugar
Diabetes meds are tools. They’re not magic. They work best when your diet supports them-not fights them.
High sugar doesn’t just make your numbers worse. It makes your meds less effective, increases your risk of side effects, and forces you into a cycle of higher doses, more complications, and more doctor visits.
The goal isn’t perfection. It’s consistency. It’s awareness. It’s choosing meals that let your medicine do its job instead of fighting against it.
Take back control-not by being perfect, but by being smart. Your blood sugar, your energy, and your future will thank you.





15 Comments
I’ve been on metformin for 5 years and the only thing that actually moved my A1c was cutting out sugary coffee drinks. I didn’t even realize how much sugar was in my ‘skinny’ latte until I started tracking. Now I drink black coffee with a splash of almond milk and my numbers are stable. It’s not about being perfect-just consistent.
So let me get this straight-eating sugar is bad? Shocking. Next you’ll tell me breathing oxygen is dangerous. I mean, I’ve been eating donuts with my metformin since 2018 and I’m still alive. Maybe the real problem is your meds suck, not my diet.
As someone who’s been managing type 2 for over a decade, I can tell you this: consistency is everything. I used to swing between zero carbs one day and pasta bombs the next. My blood sugar was a rollercoaster. Once I started eating roughly the same amount of carbs at each meal-even if it was just 40 grams-I stopped having those terrifying lows and highs. It’s not about restriction. It’s about rhythm. Your body learns the pattern, and your meds work better with it. Also, pairing fruit with nuts? Game changer. I eat an apple with almond butter every morning now. No crash, no craving, no panic.
THE PHARMA BIG SUGAR COVERUP IS REAL. They don’t want you to know that metformin was originally derived from French lilac-and now they’re pushing you to eat sugar so you need MORE drugs. And don’t get me started on Ozempic-pharma’s new profit machine. They’re selling you a magic pill while hiding the fact that your kidneys are flushing out glucose like it’s a detox. They don’t care if you gain weight back once you stop. They just want your subscription. Wake up. Read the studies. The FDA is complicit. #SugarIsTheNewCigarette
People in America think they can fix diabetes with just food swaps and apps. In India, we’ve been managing this for generations with simple things: millet roti, bitter gourd curry, no sugar in tea. You don’t need a dietitian-you need to go back to your roots. Your ancestors didn’t have glucose monitors, but they didn’t have diabetes either. Stop listening to Western influencers and eat real food. No more white rice. No more soda. Eat like your grandparents did. That’s the real medicine.
There is no such thing as 'moderation' when it comes to sugar and diabetes. The data is unequivocal. The American Diabetes Association’s guidelines are compromised by industry influence. If you are taking insulin secretagogues and consuming inconsistent carbohydrate loads, you are endangering your life. This is not a lifestyle choice. It is a medical imperative.
I’ve been on metformin for 3 years and honestly, I didn’t get it until I started eating more fiber. I used to eat white rice with every meal. Then I switched to brown rice and added lentils. My post-meal spikes dropped like a rock. I didn’t even cut sugar-I just slowed it down. It’s not about banning things. It’s about how you eat them. Also, walking 20 minutes after dinner? Huge help. No magic, just science.
Bro I just started Ozempic and I’m already losing weight 😎 But I still had a slice of cake last night… and guess what? My glucose was still under 140! So yeah, maybe the meds DO work? 🤷♂️ #OzempicLife #DiabetesWin
You got this. I was where you are-overwhelmed, confused, scared. But one small change at a time? That’s how you win. Swap one soda for sparkling water. Add a handful of almonds to your snack. Ask your doc for that dietitian referral. You don’t have to be perfect. You just have to show up. And you’re already doing that by reading this. That’s huge. Keep going. 💪
Let’s be clear: the medical establishment has turned diabetes into a cash cow. They profit from your dependence on drugs, your confusion, your guilt. They don’t want you to heal-they want you to maintain. And they’ve weaponized nutrition advice to keep you dependent. This article is just another layer of the scam. Real healing? Fasting. Ketosis. Intermittent fasting. Not ‘swap your yogurt.’ That’s corporate wellness theater.
My mom went from 9.2 A1c to 6.1 in 8 months just by eating carbs with protein. No fancy diet. No supplements. Just eggs with her toast. She says it’s the simplest thing she’s ever done. I cried reading this. I’m gonna try it tomorrow.
From India to the US-this message is universal. Sugar is the silent enemy. I work with diabetic patients daily. The ones who succeed? They don’t follow trends. They follow rhythm. Same carbs. Same time. Same protein. That’s it. Also, walking after meals is the cheapest, most effective drug out there. I tell everyone: 15 minutes. Right after eating. You’ll be shocked. 🙏
The notion that medication can compensate for dietary chaos is a metaphysical error. The body is not a machine that can be calibrated with pharmacological inputs alone. Metformin modulates hepatic glucose production, but it cannot transcend the thermodynamic reality of excessive carbohydrate influx. The body seeks homeostasis; when presented with chronic glycemic overload, it adapts through resistance-not compliance. Thus, the pharmacological intervention becomes an increasingly inadequate proxy for metabolic integrity. We are treating symptoms, not restoring function.
While the article correctly identifies the deleterious impact of added sugars on pharmacokinetics, it fails to contextualize the epistemic limitations of glycemic index as a metric. The GI is a population-based average that ignores interindividual variability in insulin sensitivity, gut microbiota composition, and postprandial lipid flux. Furthermore, the conflation of ‘low-GI’ with ‘health-promoting’ is a reductionist fallacy. A serving of lentils may have a low GI, but its phytate content can impair micronutrient bioavailability. The real solution lies in personalized metabolic phenotyping-not dietary dogma.
Interesting. I’ve been on metformin for 10 years. My sugar is fine. I eat what I want. Maybe it’s genetics. Or maybe I just don’t stress about it. Not everyone needs to follow the same rules.