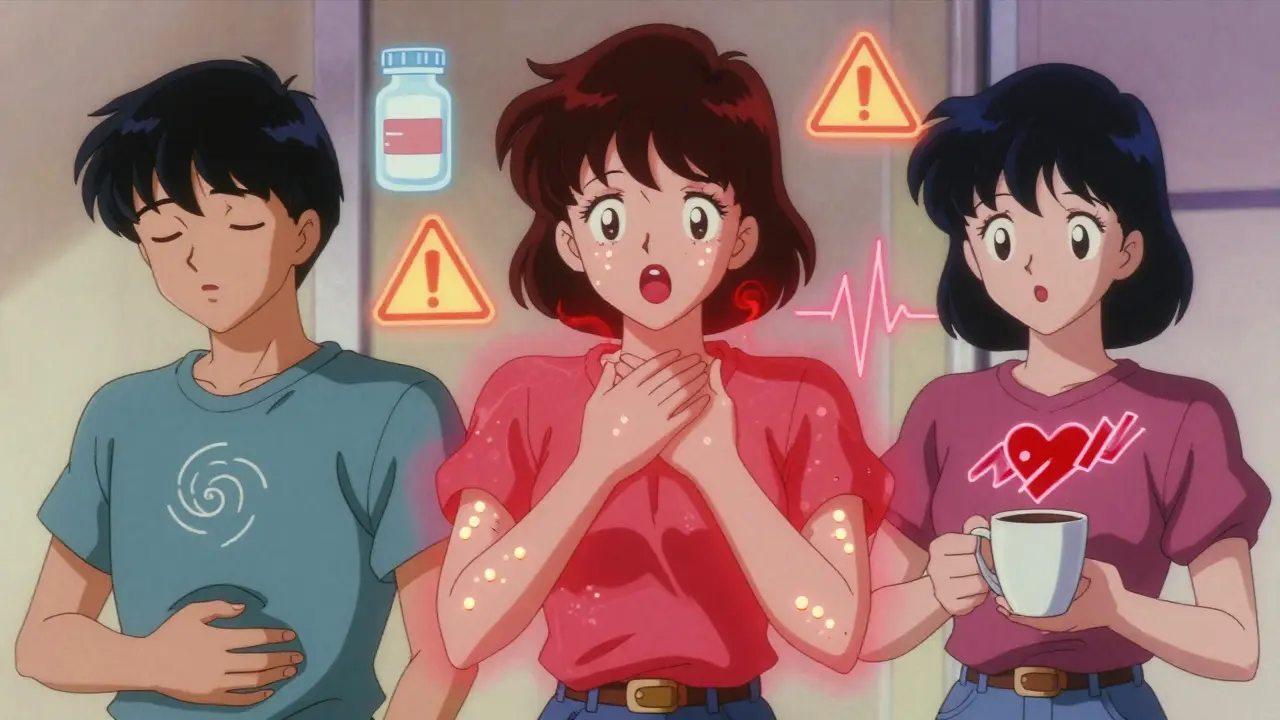
You took a pill, and now you feel sick. Maybe your stomach churns. Maybe your skin itches. Maybe you’re short of breath. You panic and tell your doctor, "I’m allergic to this." But here’s the truth: most people who think they’re allergic to a medication aren’t. In fact, up to 90% of reported drug "allergies" are actually side effects or intolerances. And that mistake can cost you - not just in money, but in health.
What’s Really Happening When You React to a Drug?
Not all bad reactions are the same. There are three very different things that can happen after you take a medicine: side effects, allergic reactions, and intolerance. Each has its own cause, timing, and risk. Mixing them up leads to wrong decisions - like avoiding a life-saving antibiotic because you got nauseous once.Let’s break it down simply.
Side Effects: The Expected Unwanted Bonus
Side effects are predictable. They’re built into how the drug works. Think of them as the price you pay for the benefit. If a drug blocks pain signals, it might also slow your digestion. If it calms your brain, it might make you drowsy.These aren’t rare. The American Society of Health-System Pharmacists lists over 15,000 documented side effects across common medications. Here’s what they look like in real life:
- Nausea and diarrhea from NSAIDs like ibuprofen (affects 25-30% of users)
- Dizziness or fatigue from SSRIs like sertraline (15-20% of users)
- Sleepiness from first-generation antihistamines like diphenhydramine (up to 40% of users)
Key signs it’s a side effect:
- Happens at normal doses
- Gets better or goes away after a few days
- Gets worse if you take more
- Doesn’t involve swelling, breathing trouble, or hives
Doctors can often fix these. Take metformin with food? Reduces stomach upset in 60% of people. Switch to a different time of day? Might cut dizziness. A lower dose? Often helps.
Allergic Reactions: Your Immune System Going Haywire
An allergic reaction is your body’s immune system treating the drug like an invader. It’s not about the drug’s chemistry - it’s about your body’s response. This is rare. Only 5-10% of all bad drug reactions are true allergies, according to the American Academy of Allergy, Asthma, and Immunology.But when it happens, it can be serious - even deadly.
True allergic reactions usually show up fast - within minutes to an hour. Symptoms include:
- Hives (raised, itchy red welts)
- Swelling of the lips, tongue, or throat (angioedema)
- Wheezing or trouble breathing
- Drop in blood pressure, dizziness, fainting
- Anaphylaxis - a full-body emergency that needs epinephrine right away
Some reactions are delayed - like a rash that appears 2-5 days later. That could be DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms), a rare but dangerous condition with a 10% death rate if untreated.
Here’s the catch: if you’ve had one true allergic reaction, you’re at higher risk for another. And you’ll likely need to avoid not just that drug, but others in the same family. For example, if you’re allergic to penicillin, you might also react to amoxicillin or cephalosporins.
But here’s the bigger problem: most people who say they’re allergic to penicillin aren’t. The CDC says 10% of Americans think they are. But when tested, only 1% actually are. That means 9 out of 10 people are avoiding a safe, cheap, effective antibiotic - and getting stronger, riskier ones instead. That increases their chance of getting a deadly infection like C. diff or MRSA by 30-50%.
Intolerance: Too Much of a Good Thing
Intolerance is the gray zone. It’s not an allergy. It’s not a classic side effect. It’s your body being unusually sensitive to a drug’s normal action.Think of it like this: most people can drink two cups of coffee without shaking. But one person gets a racing heart, sweating, and panic from just one. That’s not an allergy to caffeine - it’s intolerance.
Same with medications:
- Some people get severe nausea from codeine - not because it’s toxic, but because their body turns it into morphine too fast (ultra-rapid metabolizers). This affects about 7% of Caucasians.
- People with asthma might get wheezing from aspirin or ibuprofen (aspirin-exacerbated respiratory disease). That’s not an allergy - it’s intolerance. They can often take celecoxib (a COX-2 inhibitor) without issues.
- Some people get migraines from nitrates in processed meats or medications - not because they’re allergic, but because their blood vessels react strongly.
Intolerance is often genetic. It’s tied to how your body processes the drug - enzymes, receptors, metabolism. Unlike allergies, it doesn’t involve antibodies or immune cells. That’s why you might tolerate a drug at a lower dose, or switch to a similar one.
How to Tell Them Apart: A Quick Guide
Here’s how to spot the difference in real time:| Feature | Side Effect | Allergic Reaction | Intolerance |
|---|---|---|---|
| Cause | Drug’s normal action | Immune system overreaction | Body’s unusual sensitivity |
| Timing | Hours to days after starting | Minutes to 1 hour (immediate) or 2-5 days (delayed) | Usually within hours |
| Key Symptoms | Nausea, dizziness, dry mouth, fatigue | Hives, swelling, wheezing, low blood pressure | Exaggerated version of side effect (e.g., extreme nausea, asthma flare) |
| Repeats with dose? | Yes, often worse with higher dose | Yes, and can get worse each time | Yes, but may be dose-dependent |
| Can you try again? | Yes, often with adjustment | No - avoid completely | Maybe - try lower dose or alternative |
| Testing available? | No | Yes - skin test, blood test, oral challenge | Usually no specific test - diagnosis by elimination |
Why This Matters More Than You Think
Getting this wrong isn’t just confusing - it’s dangerous.People labeled with a "penicillin allergy" - even incorrectly - are:
- 30% more likely to get a C. diff infection
- 50% more likely to get MRSA
- Given costlier, broader-spectrum antibiotics
- More likely to have surgical infections
That’s not just theory. A 2022 study across 127 U.S. hospitals showed that when hospitals started routinely testing patients for penicillin allergy, they cut broad-spectrum antibiotic use by 35% and shortened hospital stays by over a day.
And the financial cost? The Agency for Healthcare Research and Quality estimates penicillin allergy mislabeling alone costs the U.S. system $1.2 billion every year.
What Should You Do?
If you’ve had a bad reaction to a drug, don’t just label it "allergy." Ask yourself:- Did I get hives, swelling, or trouble breathing?
- Did it happen within an hour of taking the drug?
- Did I need epinephrine or a trip to the ER?
If yes - you may have a true allergy. See an allergist.
If no - it’s probably a side effect or intolerance. Talk to your doctor about:
- Could this be fixed with a lower dose?
- Is there a similar drug I might tolerate better?
- Should I get tested to confirm?
For penicillin and other common antibiotics, testing is simple. It’s a skin test and a small oral challenge - both safe and quick. Many clinics now offer this as routine care.
And if you’ve been avoiding a drug for years because of a stomach upset or headache? You might be safe to try it again - under supervision.
What to Tell Your Doctor
Stop saying, "I’m allergic to this." Start saying:- "I got nausea and diarrhea after taking amoxicillin. It went away after a few days."
- "My face swelled up 20 minutes after taking penicillin. I had to use an EpiPen."
- "I get bad asthma when I take ibuprofen, but I can take celecoxib fine."
Be specific. Note the timing. Describe the symptoms. Mention if you needed emergency treatment. This helps your doctor classify it correctly - and keep you safe.
What’s Changing Right Now
The medical world is catching on. The FDA now requires drug labels to clearly separate allergy risks from side effects. Hospitals are using AI tools to flag mislabeled allergies in electronic records. New point-of-care penicillin tests are being developed that give results in 15 minutes instead of 3 hours.And the big win? A simple clinical tool called PEN-FAST, currently being tested, could let doctors safely clear 90% of people who think they’re allergic - without any testing at all. Results are expected in mid-2025.
This isn’t just about avoiding a rash. It’s about getting the right medicine - safely, quickly, and without unnecessary risk.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Up to 80% of people who had a true penicillin allergy in childhood lose it over 10 years. That’s why testing later in life is so important - you might be able to safely use it again.
If I’m allergic to one NSAID, am I allergic to all of them?
Not necessarily. True NSAID allergy is rare and usually specific to one drug. But NSAID intolerance - which causes asthma or hives - often affects all COX-1 inhibitors like ibuprofen and naproxen. You might still tolerate celecoxib, which works differently. An allergist can test this.
Is a rash always an allergy?
No. Many rashes from drugs are side effects - especially if they’re mild, itchy, and appear days after starting the medicine. A true allergic rash is often raised, red, and spreads quickly. Delayed rashes like DRESS are serious and need urgent care. Only a doctor can tell the difference.
Can I test myself at home for a drug allergy?
Never. Self-testing can trigger a life-threatening reaction. Skin tests and oral challenges must be done under medical supervision with emergency equipment on hand. If you’re unsure, see an allergist - don’t guess.
What should I do if I think I had an allergic reaction?
If you had swelling, trouble breathing, or passed out - go to the ER immediately. After that, ask for a referral to an allergist. Bring your medical records. Don’t assume you’re allergic - get tested. That one step could save your life next time you need antibiotics.
Next Steps: What to Do Today
If you’ve ever said, "I’m allergic to this drug," here’s what to do now:- Check your medical records. What exactly was written down? "Allergy"? Or "nausea"?
- If it’s just nausea, dizziness, or diarrhea - talk to your doctor about whether it’s really an allergy.
- If you had swelling, hives, or breathing trouble - schedule an allergist appointment.
- If you’re scheduled for surgery or need antibiotics - ask if you’ve been wrongly labeled.
- Update your records. Don’t let a 10-year-old stomach upset keep you from safe, effective treatment.
Medicines save lives. But only if you’re using the right one. Getting the difference right isn’t just smart - it’s essential.





15 Comments
So let me get this straight - 90% of people think they’re allergic to penicillin but they just got a tummy ache? And we’re all still getting prescribed $500 antibiotics because someone once said 'it made me feel weird'? 😒
It is imperative to underscore the clinical significance of distinguishing between pharmacological side effects, immunoglobulin E-mediated hypersensitivity reactions, and non-immunologic intolerances. Misclassification not only compromises therapeutic efficacy but also contributes to antimicrobial resistance on a systemic level. The data cited herein is both robust and compelling.
People just don't understand medicine is not a menu you pick and choose from your comfort zone your body has to adapt or get left behind
OMG YES THIS!! I’ve been telling my doctor for YEARS that ibuprofen gives me a headache and she just kept saying ‘it’s a side effect’ like I’m making it up 😤 Turned out I’m intolerant - celecoxib saved my life. Why isn’t this common knowledge??
In the United States, the issue of drug allergy mislabeling has become a public health crisis with profound implications for antibiotic stewardship. The CDC estimates that approximately 10% of the population carries a penicillin allergy label, yet fewer than 1% are confirmed allergic upon testing. This misclassification leads to increased use of broad-spectrum agents such as vancomycin and fluoroquinolones, which in turn elevates the risk of C. difficile infection, MRSA colonization, and Clostridioides difficile recurrence. Hospitals that have implemented formal penicillin allergy de-labeling programs report reductions in inappropriate antibiotic use by 30-40%, decreased lengths of stay, and lower healthcare costs. The PEN-FAST clinical decision tool, which is currently undergoing validation, may soon enable primary care providers to safely de-label up to 90% of patients without requiring formal allergy testing - a paradigm shift that could redefine outpatient care.
I knew it. Big Pharma and the AMA are keeping this quiet because they make BILLIONS off unnecessary antibiotics. You think this is about health? Nah. It’s about profit. They don’t want you to know you can just take a lower dose or switch to celecoxib. They want you dependent on their $800 pills. #PharmaLies
The DRESS syndrome? That’s not a rash. That’s your immune system staging a coup. And if you think you’re just ‘sensitive’ to a drug, you’re one pill away from multi-organ failure. This isn’t ‘oh I got a little itchy’ - this is ‘I woke up with my skin peeling off’ territory. Stop normalizing the dangerous.
I appreciate the nuance here. I used to think my nausea from metformin meant I was allergic - turned out it was just taking it on an empty stomach. Now I take it with dinner and feel fine. Sometimes the fix is that simple. Thanks for clarifying the difference - this should be taught in high school.
this is so helpful i always thought if i felt bad after a pill it was an allergy but now i know to check the timing and symptoms before panicking
I’m so glad someone finally broke this down! I had a rash after amoxicillin when I was 8 - got labeled allergic forever. At 32, I got tested and turned out I’m fine. Now I can take penicillin for my pneumonia and save $2000. This info? LIFE CHANGING.
I love how this doesn’t just dump facts - it gives you a lens. Side effects? The price of admission. Allergy? The system’s alarm going off. Intolerance? Your body’s unique playlist. It’s not just medical - it’s personal. And if you’ve been avoiding a drug because of a 10-year-old stomach ache? You might be denying yourself the perfect treatment. That’s not just a mistake - it’s a tragedy waiting to happen.
I’ve been a nurse for 15 years, and I’ve seen so many patients avoid life-saving meds because they said ‘I’m allergic’ to something that was just nausea. This post is exactly what we need more of - clear, accurate, and kind. Thank you.
i had a rash after amoxicillin and now i cant take any antibiotics and i hate it but i dont wanna die so i just deal
This is all a distraction. The real issue? The FDA, CDC, and Big Pharma are using this ‘penicillin allergy’ myth to push monoclonal antibodies and AI-driven diagnostics. They want you dependent on expensive tech, not cheap pills. The 90% statistic? Fabricated. The real reason you get C. diff? Your gut was wiped out by glyphosate in your food. This whole thing is a cover-up.
They don’t want you to know that your body’s reaction to drugs is being manipulated by electromagnetic frequencies from 5G towers. The immune system is being confused by radio waves - that’s why your ‘allergy’ appears only after you’ve been near a cell tower. The FDA knows. The WHO knows. But they won’t tell you because the pharmaceutical industry owns the grid. Get tested? No. Get shielded. Buy the Faraday hat. Your life depends on it.