
Going from hospital to home should feel like relief-not a minefield. For seniors on multiple medications, one wrong pill, one missed dose, or one misunderstood instruction can lead to a fall, a trip to the ER, or even a return to the hospital. In fact, medication errors happen in nearly 1 in 5 older adults within three weeks of leaving the hospital, according to research from the Journal of General Internal Medicine. These aren’t just mistakes-they’re preventable crises.
Why Medication Errors Happen at Discharge
It’s not because doctors or nurses are careless. The problem is systemic. Hospitals discharge patients faster than ever. Paperwork piles up. Medication lists get lost between departments. Patients are tired, confused, or overwhelmed. And often, the list they leave with doesn’t match what they were actually taking before they got admitted. A 2020 AHRQ report found that hospitals using basic discharge processes have only a 60-70% accuracy rate on medication lists. But those using structured reconciliation? They hit 95%. That’s the difference between safety and danger. Common errors include:- Prescribing a drug that interacts with something the patient already takes
- Forgetting to discontinue a medication no longer needed
- Changing the dose without explaining why
- Leaving out over-the-counter pills, vitamins, or herbal supplements
The Five Steps of Medication Reconciliation
Medication reconciliation isn’t just a form to check off. It’s a process-and it has five non-negotiable steps.- Verification: Gather every medication the patient was taking before admission. This includes prescriptions, OTC drugs, patches, inhalers, and even herbal teas. Ask: “What do you take every day? What did you take last week?” Don’t trust memory alone. Bring the actual bottles.
- Clarification: Does each drug still make sense? Is the dose right? Is it still needed? For example, if someone was on a painkiller for surgery but now has no pain, it should be stopped.
- Reconciliation: Compare the admission list, current list, and discharge list. Any mismatch? Fix it. Document why.
- Communication: Send the final, accurate list to the patient’s primary care doctor, pharmacist, and home health provider. No more guessing.
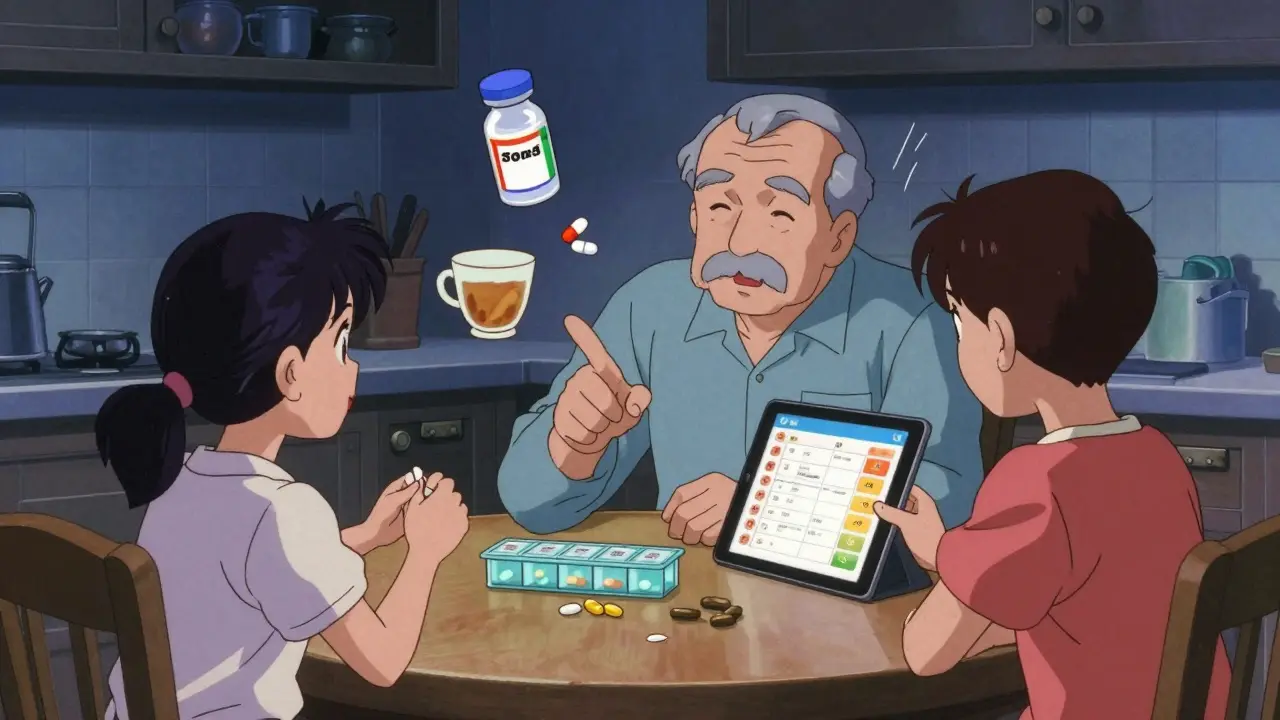
- Education: This is the most important step-and the one most often skipped. Use the Teach-Back method. Don’t just hand them a sheet. Ask: “Can you tell me how and why you take each of these pills?” If they can’t, you haven’t done your job.
Who Should Be Involved
This isn’t just the doctor’s job. It’s a team effort.- Pharmacists: They’re the experts. A 2018 JAMA study showed pharmacist-led discharge reviews cut medication discrepancies by 67%. They spot interactions, dosage errors, and redundant prescriptions no one else catches.
- Nurses: They’re the ones who talk to patients daily. They can notice confusion, dizziness, or hesitation when meds are discussed.
- Family members or caregivers: They’re often the ones who actually give the pills. They need to be in the room during the explanation.
- Home health nurses: They should do their own reconciliation within 24 hours of entering the home. Don’t assume the hospital got it right.
What to Do Before Leaving the Hospital
Don’t wait until discharge day. Start early.- Ask for a Brown Bag Medication Review during your hospital stay. Bring all your pills-even the ones in the back of the cabinet. Let the pharmacist check them against the hospital’s list.
- Request a written discharge summary that includes: drug names, doses, times, reasons, and what to watch for.
- Confirm the pharmacy you’ll use. If you’re switching from your usual pharmacy, make sure they have your full history.
- Ask: “Will someone call me within 48 hours after I get home?” Follow-up is critical.
What to Do After You Get Home
Leaving the hospital is just the beginning.- Within 24 hours, have a family member or home nurse compare the discharge list with the actual pills in the house. Use the Brown Bag method again.
- Set up a pill organizer with clear labels. Color-coded or digital reminders help seniors who forget.
- Use a medication tracker app. A 2023 JAMA Network Open study found that seniors using visual schedule apps had 41% fewer errors.
- Call your pharmacist with questions. They’re paid to answer them. Don’t be shy.
- Watch for red flags: dizziness, confusion, rash, nausea, unusual fatigue. These could mean a bad interaction or wrong dose.
- Schedule a follow-up with your doctor or pharmacist within 7 days. For high-risk patients, it’s not optional-it’s lifesaving.

Technology That Helps
You don’t need fancy gadgets-but some tools make a big difference.- Electronic Health Records (EHRs): Hospitals using integrated systems like Epic have seen medication errors drop by 28%. But only 35% of U.S. hospitals can share data with outpatient providers. If yours can’t, insist on a printed list.
- Telehealth visits: A 2021 JAMA study showed telehealth check-ins boosted medication adherence by 22%. A quick video call can catch problems before they escalate.
- AI tools: Systems like MedAware analyze prescriptions for errors and flag risks. While not yet standard, they’re growing fast.
What to Do If You’re Still Confused
If you’re unsure about a medication, don’t guess.- Call the hospital’s discharge nurse or pharmacist. They’re obligated to help.
- Go to your local pharmacy. Ask for a free medication review. Most offer it.
- Use the National Council on Aging’s Medication Safety Checklist-it’s free and easy to use.
- If you’re on Medicare, you can get Transition Care Management (TCM) services. These are covered if you’re discharged to home and need follow-up within 14 days. Ask your doctor to bill for codes 99495 or 99496.
The Bottom Line
Medication errors after hospital discharge are common-but they’re not inevitable. The fix isn’t expensive. It’s simple: involve the right people, use proven steps, and make sure the patient understands. For seniors, the stakes are high. But with the right process, you can go home safely-and stay there.What is the most common cause of medication errors after hospital discharge?
The most common cause is incomplete or inaccurate medication reconciliation. Many hospitals don’t verify what the patient was actually taking before admission, or they forget to include over-the-counter drugs, supplements, or patches. Studies show up to 76% of discharge lists still have clinically significant errors when independently checked.
Who is most at risk for medication errors after leaving the hospital?
Seniors taking five or more medications (polypharmacy), those with kidney problems, dementia, or multiple chronic conditions like heart failure or diabetes are at highest risk. Medicaid patients also face 37% more discrepancies than privately insured patients due to fragmented care systems.
Why is the Teach-Back method so important?
Teach-Back means asking the patient to explain their medications in their own words. If they can’t, they don’t understand. A 2012 study found this method improves medication adherence by 32%. For seniors, it’s not just about remembering names-it’s knowing why each pill matters and what to watch for.
Can I trust the discharge medication list I’m given?
Not without verification. Even in top hospitals, discharge lists often don’t match what patients were actually taking. Always do a Brown Bag Review-bring all your pills to your first appointment and compare them side by side with the list. Never assume it’s correct.
What should I do if I notice a mistake in my medication list after I get home?
Call your pharmacist or primary care provider immediately. Don’t stop or change anything on your own. Keep taking your meds as instructed until you get clarification. Write down the error and when you noticed it. This helps them fix it faster and prevents future mistakes.
Are there free resources to help manage medications at home?
Yes. The National Council on Aging offers a free Medication Safety Checklist. Many pharmacies offer free medication reviews. Medicare also covers Transition Care Management services if you need follow-up within 14 days of discharge. Ask your doctor if you qualify.
How can I make sure my home health nurse knows my meds?
Before they arrive, give them a printed copy of your current medication list and your Brown Bag inventory. Ask your hospital to send the official discharge summary to their agency. If they don’t ask for it, call them and send it yourself. Home health nurses must reconcile meds within 24 hours of starting care-don’t let them skip it.





8 Comments
Let’s be real-most hospitals treat medication reconciliation like a box to check off during a 12-minute discharge huddle. I’ve seen charts where ‘aspirin 81mg daily’ was listed as ‘aspirin 325mg PRN’-and the patient had been on 81mg for 12 years. The system isn’t broken; it’s intentionally under-resourced. Pharmacist-led reconciliation? Great in theory. In practice, most hospitals don’t even have a pharmacist on the discharge team. You think this is about safety? Nah. It’s about reducing bed days and hitting CMS benchmarks. The patient? Just a number in the discharge queue.
This is such an important post. I work with elderly clients, and I’ve seen too many come home with stacks of new pills and zero idea why they’re taking them. The Teach-Back method? It’s simple, but it works. I always ask my clients to show me their pill organizer and tell me what each one does. If they hesitate, we go back. No rush. Better safe than sorry. And yes-bring the brown bag. Always.
Oh sweetie, you really think the hospital gave you the right list? 😒 Honey, they didn’t even know your cat was on prednisone. I had a neighbor who took her entire medicine cabinet-17 bottles-to the ER because her discharge list left out her thyroid med AND her ‘herbal heart tonic’ (aka that weird tea her aunt swears by). They gave her a new script for a beta-blocker… that she’d been off for 3 years. 🤦♀️
While the systemic issues are undeniable, I appreciate the structured approach outlined here. The five-step reconciliation model is evidence-based and replicable across care settings. What’s often overlooked is the role of digital health literacy-many seniors don’t know how to use apps or access EHR portals. A printed, signed, and dated medication list-hand-delivered to the primary care provider-is still the gold standard. Technology helps, but human verification remains irreplaceable.
Are you telling me they don’t have a central database?!! The government has satellites that can see your face through a window, but they can’t link your hospital meds to your pharmacy?!! This is a conspiracy!! I’ve been saying for YEARS-Big Pharma and the AMA are pushing polypharmacy to keep seniors dependent!! And now they’re letting nurses rush discharges so they can get paid for ‘readmission prevention’ while you’re left confused with 14 different pills that make you dizzy!! I’ve got 17 screenshots of my mom’s med list changing every day!! I’m filing a complaint!!
Oh, this is just typical American healthcare chaos. In the UK, we have NHS pharmacists who walk patients through their meds before discharge-no exceptions. Here? You get a 2-page printout written in font size 6, and you’re expected to ‘self-manage’? Please. We have a National Health Service because we believe people deserve to be cared for, not discarded after 3 days with a clipboard and a smile. Shameful. Absolute shame. And don’t get me started on those ‘teach-back’ videos-what’s the point if your GP doesn’t even have your file?
My grandma got discharged last month with a new blood thinner, and the nurse didn’t even mention the bleeding risk. I had to call the pharmacy myself. But here’s the thing-it’s not all doom and gloom. When we used the Brown Bag method and sat down with her pharmacist for 45 minutes? She finally understood why she was on each pill. She even started using the app you mentioned. It’s not perfect, but small steps matter. If you’re reading this and you’re helping someone? Do the brown bag. Do the teach-back. It’s not extra work-it’s life-saving.
THIS. IS. EVERYTHING. 🙌 I’m a nurse, and I’ve seen it all. One guy got discharged with 12 meds-he was only on 5 before. He took the extra 7 and ended up in the ER with a heart attack. 😭 But here’s the good part: we started doing team huddles before discharge-pharmacist, nurse, family, patient. Now our error rate’s down 80%. 🚀 So yes, it’s broken… but we can fix it. One brown bag at a time. 💪❤️