
Fulminant Hepatic Failure Risk Assessment
Fulminant Hepatic Failure Risk Assessment
This tool helps identify potential signs of fulminant hepatic failure based on medication use and symptoms. Early recognition is critical - survival rates jump from 28% to 63% when caught before complete liver failure.
Important: This tool is for informational purposes only. Fulminant hepatic failure is a medical emergency. If you or someone you know has these symptoms, seek emergency medical care immediately.
Disclaimer: This assessment is not a substitute for professional medical advice. Always consult with a healthcare provider for proper diagnosis and treatment.
What Is Fulminant Hepatic Failure?
Fulminant hepatic failure (FHF), also called acute liver failure, happens when a healthy liver suddenly stops working-often in just days. It’s not something that creeps up slowly. It strikes fast. People with no prior liver problems can go from feeling mildly sick to confused, bleeding uncontrollably, and slipping into coma. The key signs? Yellow skin (jaundice), mental changes like confusion or drowsiness (hepatic encephalopathy), and blood that won’t clot (coagulopathy). Without quick action, death can follow within hours.
This isn’t rare. In the U.S., about 2,000 cases happen every year. And nearly half of them? Caused by medications. That includes common painkillers, antibiotics, herbal supplements-even things you buy over the counter. The word "fulminant" comes from Latin, meaning "to strike like lightning." That’s exactly what it does.
Acetaminophen: The Silent Killer
Acetaminophen (Tylenol) is the single biggest cause of fulminant hepatic failure in the U.S., responsible for nearly 46% of all drug-induced cases. People think it’s safe because it’s in so many medicines. But taking too much-even if it’s "just" the recommended dose-can be deadly.
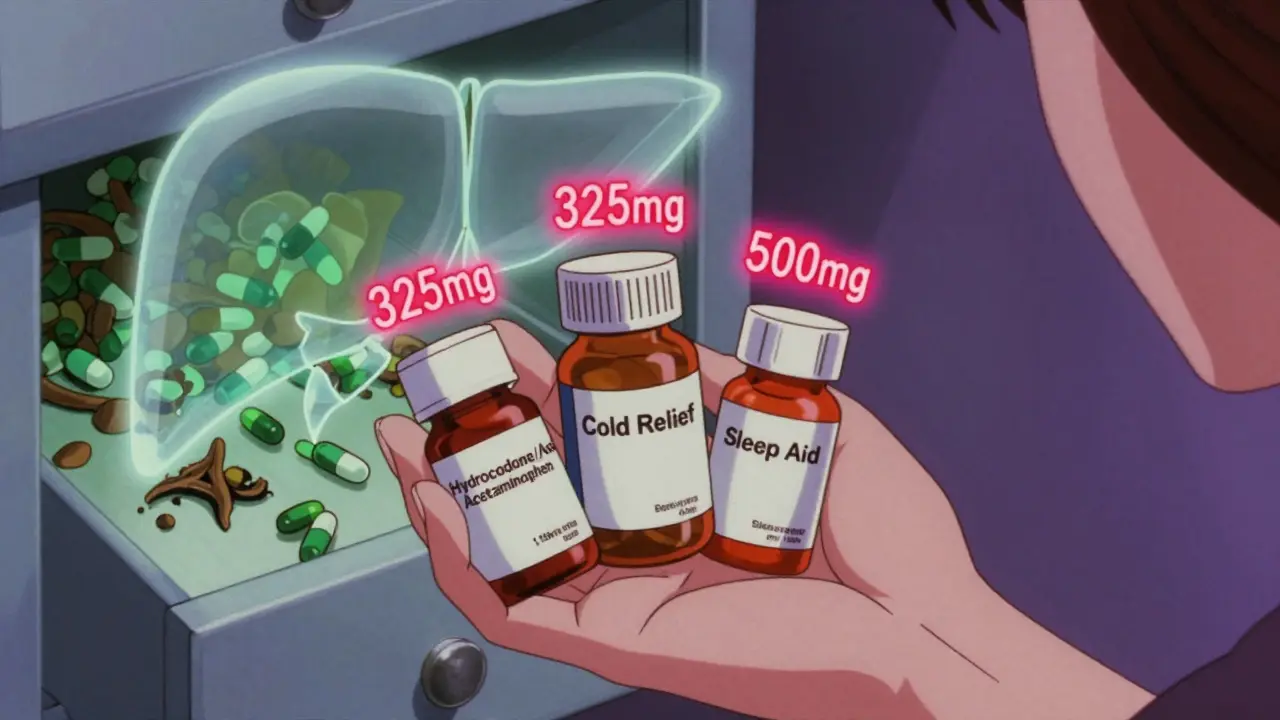
Here’s the scary part: if someone takes more than 7.5 grams in one day (or 150 mg per kg of body weight), their liver starts dying. That’s not even a huge amount. It’s just 10 extra 500 mg pills. Many people don’t realize they’re overdosing because they’re taking multiple medicines that all contain acetaminophen-like cold pills, sleep aids, or prescription painkillers like hydrocodone/acetaminophen. One patient in a 2022 Johns Hopkins case series was taking three different prescriptions, each with acetaminophen. She thought she was safe. Her liver failed in 72 hours.
The biochemical clue? ALT levels above 1,000 IU/L. That’s 20 times the normal range. And if the ALT is more than twice the AST, that’s a classic acetaminophen signature. But here’s what most ERs miss: 23% of patients with acetaminophen-induced liver failure say they didn’t take any extra pills. They’re not lying. They just didn’t know the total amount they were consuming.
Other Medications That Can Destroy the Liver
Acetaminophen isn’t the only culprit. Antibiotics like amoxicillin-clavulanate (Augmentin) can cause liver failure, but they don’t act fast. It often takes weeks of use before symptoms show up. And when they do, it looks like a bad case of the flu-fatigue, nausea, dark urine. But the liver enzymes tell a different story: alkaline phosphatase more than double the normal level, and jaundice lasting longer than 18 days.
Antiseizure drugs like valproic acid are another hidden danger. They cause a rare but deadly condition called microvesicular steatosis. Before encephalopathy hits, ammonia levels spike above 150 μmol/L. That’s a red flag. But many doctors don’t check ammonia unless they’re thinking of kidney failure or sepsis.
Herbal supplements are the fastest-growing cause. Green tea extract, kava, and certain weight-loss products have been linked to liver failure. One 2022 study found that 42% of herbal supplement cases involved green tea extract taken at doses over 800 mg per day. People think "natural" means safe. It doesn’t. A woman in Florida took 3,000 mg of kava daily for six months to treat anxiety. She showed up in the ER with grade IV encephalopathy and an INR of 5.8. She needed a transplant.
How to Spot It Before It’s Too Late
Early recognition saves lives. Survival jumps from 28% to 63% if you catch it before the liver shuts down completely. So what should you look for?
- Jaundice + nausea: If someone has yellow eyes or skin and has been vomiting for more than 24 hours, get an ALT and INR test-right away.
- Personality changes: Family members often notice subtle shifts: confusion, forgetfulness, irritability, or even sleepiness. These aren’t "just stress." They’re signs of brain swelling from liver failure.
- INR above 1.5: This is the single most important lab value. If it’s above 1.5, the liver can’t make clotting factors. If it hits 6.5, mortality without transplant is 90%.
- Acetaminophen level: Test it in EVERY patient with ALT over 500 IU/L-even if they deny taking it. That’s the AASLD guideline. And if the level is above 150 μg/mL at 4 hours after ingestion, the risk of liver damage is 60%.
Don’t wait for the classic triad. By the time jaundice, encephalopathy, and coagulopathy are all present, it’s often too late. The earlier you test, the better the chance.
The Emergency Protocol: What Hospitals Must Do
Time is liver. The Acute Liver Failure Study Group recommends a 30-minute emergency triage protocol:
- Check ALT, INR, and acetaminophen level immediately in anyone with nausea/vomiting plus jaundice.
- Assess mental status every hour using the West Haven Criteria. Grade III or IV encephalopathy means transplant is likely needed.
- Repeat INR every 6 hours if it’s above 1.5. Rising INR = worsening prognosis.
If acetaminophen is involved, give N-acetylcysteine (NAC) within 8 hours. It’s not just helpful-it’s life-saving. Even if the patient denies taking it, give NAC anyway. The risk of giving it is near zero. The risk of not giving it? Death.
For non-acetaminophen cases, the King’s College Criteria determine transplant eligibility: INR over 6.5 with encephalopathy, or pH below 7.3 with high creatinine. These aren’t suggestions. They’re thresholds. Cross them, and transplant is the only option.
What Goes Wrong in Real Life
Doctors aren’t ignoring this. They’re missing it.
A nurse practitioner in Ohio reported a case where a 45-year-old woman on 4 grams of acetaminophen daily for back pain showed up confused. The ER team checked her glucose, did a CT scan for stroke, and didn’t test her liver enzymes until she started bleeding from her gums. By then, her INR was 8.2.
Another case: a man with fever, vomiting, and jaundice was diagnosed with gastroenteritis. He was sent home with anti-nausea meds. Two days later, he was back in the ICU with liver failure. He’d been taking ibuprofen for a month. NSAIDs don’t usually cause this-but they can, especially with long-term use.
Herbal supplements are the trickiest. Patients don’t mention them. They think it’s "just tea." Or they’re embarrassed. But 42% of herbal-related liver failure cases involve green tea extract. That’s not a myth. That’s data.
What’s Changing Now
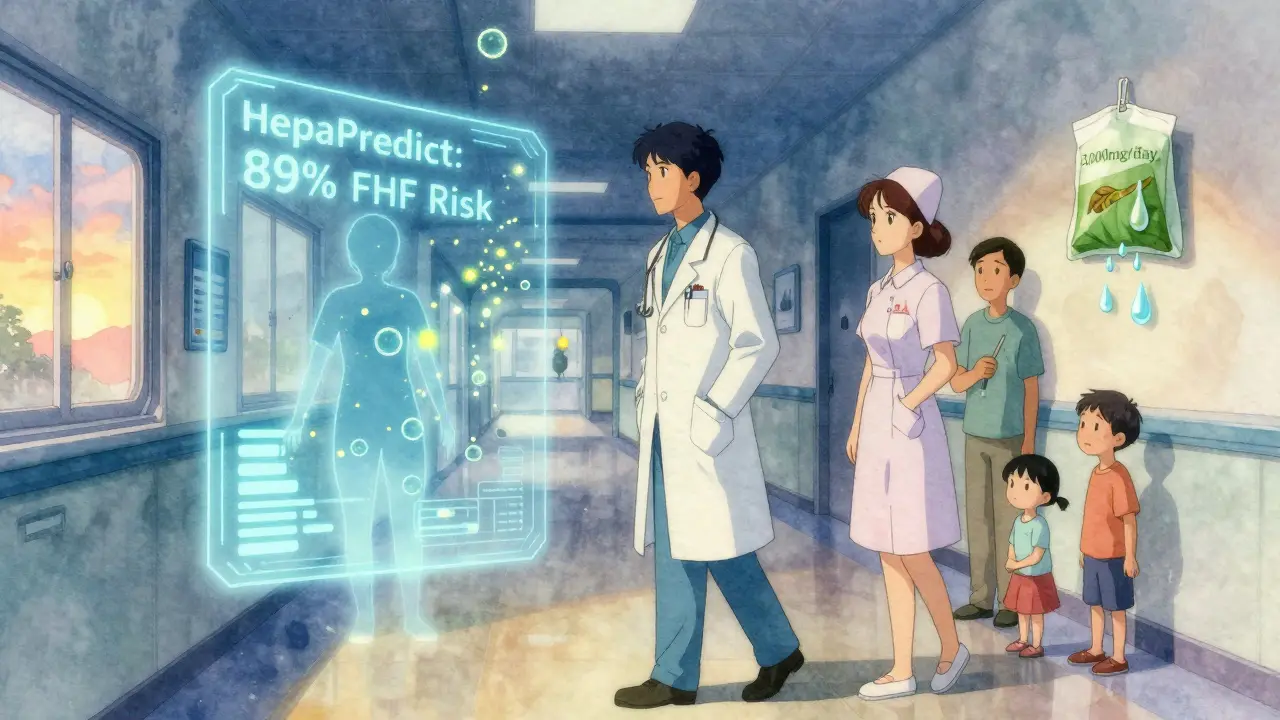
The system is getting better. In 2023, the FDA cleared HepaPredict, an AI tool that uses 17 clinical variables to predict liver failure with 89% accuracy within 24 hours. Emergency departments in California are already using it to cut transplant wait times by more than a day.
By mid-2024, a national "FHF Alert System" will require ERs to report suspected cases within one hour. That means transplant teams can start evaluating patients before they crash.
And research is moving fast. A new blood marker, miR-122, can detect acetaminophen toxicity as early as 6 hours after ingestion-before ALT even rises. That could change everything.
But the biggest problem remains: people don’t know. Doctors don’t always ask. And when they do, patients don’t tell.
What You Need to Remember
If you or someone you know has:
- Unexplained nausea and vomiting,
- Yellow skin or eyes,
- Confusion or unusual sleepiness,
- And has taken any medication-even "safe" ones-
Go to the ER. Ask for ALT, INR, and acetaminophen level. Don’t wait. Don’t assume it’s the flu. Don’t assume it’s "not serious."
Fulminant hepatic failure doesn’t wait. And neither should you.
Can you survive fulminant hepatic failure without a transplant?
Yes-but only if caught early. About 63% of people survive without a transplant if they get treated within the first 24-48 hours, especially if it’s caused by acetaminophen. N-acetylcysteine can reverse damage if given in time. But if encephalopathy is advanced or INR is above 6.5, survival without transplant drops to less than 10%.
Is acetaminophen safe if I take it as directed?
Not always. Many people exceed the safe limit without realizing it. The maximum daily dose is 4,000 mg-but that’s easy to exceed if you’re taking multiple medicines with acetaminophen, like cold pills, sleep aids, or prescription painkillers. A single prescription like hydrocodone/acetaminophen can have 325 mg per pill. Taking 12 pills in a day hits the limit. Add a Tylenol on top? You’re in danger.
Can herbal supplements cause liver failure?
Absolutely. In the U.S., herbal and dietary supplements caused 13% of all acute liver failure cases between 2019 and 2022. Green tea extract (specifically EGCG at doses over 800 mg/day), kava, and weight-loss products are the top culprits. Symptoms can take weeks to appear, so people don’t connect the dots. Women are more often affected, and many cases are misdiagnosed as viral hepatitis.
What’s the most important lab test to check in an emergency?
INR. It measures how well your blood clots. A normal INR is around 1.0. If it’s above 1.5, your liver isn’t making clotting factors. If it’s above 6.5, you’re in critical danger. Rising INR is the clearest sign that liver failure is worsening. ALT tells you the liver is damaged-but INR tells you it’s failing.
Should I get tested if I took extra acetaminophen but feel fine?
Yes-if you took more than 7.5 grams in a day, or 150 mg per kg of body weight. Liver damage can start before you feel sick. The liver doesn’t hurt until it’s severely damaged. If you’re unsure, go to the ER. A blood test takes 15 minutes. Waiting for symptoms could cost you your life.
Is there a hotline for help with suspected liver failure?
Yes. The National Acute Liver Failure Foundation runs a 24/7 hotline at 1-888-567-6253. They connect patients and ERs directly to transplant centers. Their average response time is under 18 minutes. If you suspect FHF, call them. They’ll help coordinate urgent care-even on weekends or holidays.





11 Comments
bro i took 2 tylenol for my headache last week and now i’m scared to breathe. like wtf is this article saying i could’ve been a goner? i didn’t even know my cold medicine had it in it too. 😳
This is yet another example of how the pharmaceutical-industrial complex has normalized self-annihilation through over-the-counter commodification. The biochemical markers are not merely clinical-they are ethical indictments. ALT >1000 IU/L isn't just a lab result; it's the liver screaming into a void where regulatory oversight should be. And yet, we let people walk out of pharmacies with 500mg pills like they’re M&Ms. This isn't negligence. It's systemic violence disguised as consumer freedom.
I work in a clinic and see this all the time. A woman came in last month with jaundice and confusion-she’d been taking 4 different meds with acetaminophen, including a sleep aid she got from her cousin. She didn’t think it counted because it was 'just a little extra.' We got her NAC in time. She’s fine now. But so many don’t make it. Please, if you take anything for pain or sleep-check the label. It’s not just Tylenol. It’s everywhere.
lol so the real problem is people are too dumb to read labels? i mean yeah, 7.5g is a lot but if you’re taking 10 pills of tylenol plus hydrocodone plus nyquil plus that ‘immune booster’ from gnc… you’re not a victim. you’re a walking biohazard. also green tea extract? bro that’s just concentrated caffeine with liver toxins. if you’re drinking 3000mg of kava for anxiety you’re not healing-you’re self-medicating like a caveman with a chainsaw.
I mean, I get the urgency, but this whole thing feels like fearmongering wrapped in a white coat. How many of these cases are actually *unintentional*? I bet half the people who get FHF from acetaminophen are just trying to OD and are too embarrassed to say it. And the herbal supplement stuff? Yeah, some people go full alchemist with kava, but that’s not the norm. Most people who take green tea extract are just trying to lose weight and think it’s a magic bullet. The real issue isn’t the meds-it’s the culture of quick fixes and the lack of basic health literacy. We’re treating symptoms of a societal disease, not the disease itself.
The liver doesn’t scream. It whispers. And we’ve trained ourselves to ignore whispers. We’ve turned our bodies into data points-ALT, INR, AST-while forgetting that pain is a language, and silence is the loudest symptom. When you say ‘go to the ER,’ you’re not just giving advice. You’re asking someone to surrender their autonomy to a machine that doesn’t care if they’re scared, broke, or undocumented. NAC saves lives? Sure. But who saves the people who can’t afford the ER? Who saves the ones who get sent home with anti-nausea meds because the triage nurse didn’t see the yellow eyes? This isn’t just medical. It’s moral. And we’re failing.
Ah yes, the classic ‘your Tylenol is trying to kill you’ panic. Next up: ‘your water is secretly a liver assassin.’ Look, if you’re taking 10 pills a day because you’re addicted to painkillers, maybe the problem isn’t the acetaminophen-it’s the fact that you’re using pills to numb your existence. And ‘natural’ supplements? Please. If your ‘herbal tea’ costs more than your rent and comes in a bottle with a mandala on it, you’re not healing. You’re performing wellness. Congrats. You’ve turned your liver into a TikTok aesthetic.
The article cites 42% of herbal cases involve green tea extract, yet fails to mention that 89% of those cases involve doses exceeding 1000 mg/day. The real issue is dosage toxicity, not the substance itself. EGCG is a polyphenol with biphasic effects-low doses are antioxidant, high doses are pro-oxidant. This isn't a failure of regulation; it's a failure of public education on pharmacokinetics. Also, why is there no mention of CYP450 polymorphisms? Some populations metabolize acetaminophen slower. This is reductionist.
The clinical data presented is robust and aligns with current AASLD guidelines. However, the narrative framing inadvertently reinforces a binary model of medical responsibility-either the patient is ignorant or the system is negligent. In reality, the issue lies in the fragmentation of care: primary care providers rarely screen for OTC use, ERs are overloaded, and pharmacists are underutilized as safety nets. A systemic intervention-mandatory OTC medication reconciliation at point-of-sale via pharmacy software-would reduce unintentional overdose by an estimated 37% according to a 2023 JAMA study. This is not a moral failing. It is a logistical one.
I’m a nurse. I’ve seen it. One sentence: If you’re dizzy, yellow, and took anything for pain-go now. Don’t wait. Don’t text your mom. Don’t Google it. Go.
this hit different 😔 i took tylenol for my back pain for 3 weeks straight because i didn’t wanna tell my dr i was still hurting… i didn’t even know i was overdosing. just wanted to feel normal. i’m alive bc i went in when my eyes turned yellow. pls check your meds. 💔❤️🩹