Treatment-Resistant Schizophrenia Treatment Calculator
This calculator helps you and your doctor evaluate treatment options for treatment-resistant schizophrenia by weighing the most important factors.
Your Treatment Options
Clozapine
Best effectiveness (40-60% response)
Weekly blood tests required
Olanzapine
Moderate effectiveness (25-35% response)
No special monitoring
Risperidone
Moderate effectiveness (20-30% response)
No special monitoring
Quetiapine
Moderate effectiveness (20-30% response)
No special monitoring
Aripiprazole
Mild to moderate effectiveness (15-25% response)
No special monitoring
Paliperidone
Moderate effectiveness
Monthly injection
Recommended Option
Important Note: This tool is for educational purposes only. Always consult with your psychiatrist before making treatment decisions. Clozapine requires strict medical supervision due to the risk of agranulocytosis.
When standard antipsychotics fail, doctors turn to Clozapine - a drug that works where others don’t. But it’s not simple. Clozapine saves lives, but it also demands constant blood tests, carries serious side effects, and isn’t for everyone. If you or someone you care about has tried at least two other antipsychotics without relief, you’re likely weighing Clozapine against its alternatives. This isn’t about picking the "best" drug. It’s about finding the right balance between effectiveness and safety.
Why Clozapine Is Different
Clozapine isn’t just another antipsychotic. It’s the only medication approved by the FDA and Health Canada specifically for treatment-resistant schizophrenia - meaning it’s used when at least two other drugs have failed. About 30% of people with schizophrenia don’t respond to typical antipsychotics. For them, Clozapine is often the last option. And it works. Studies show it reduces hallucinations, delusions, and suicidal behavior better than any other antipsychotic. In one large trial, nearly 50% of patients on Clozapine saw significant improvement, compared to under 20% on other drugs.
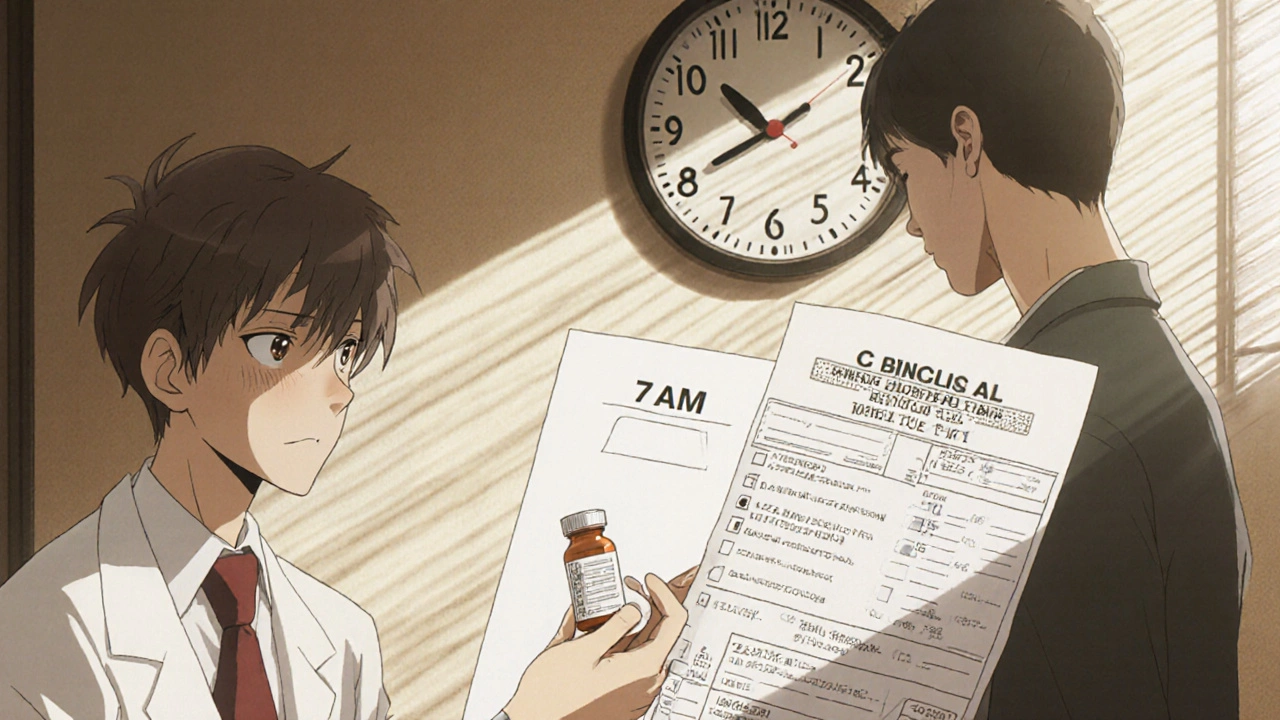
But here’s the catch: Clozapine can cause agranulocytosis - a dangerous drop in white blood cells that leaves the body vulnerable to infections. That’s why anyone taking it must get weekly blood tests for the first six months, then every two weeks after that. Missing a test means stopping the drug immediately. It’s a heavy burden, but for many, the trade-off is worth it.
Common Alternatives to Clozapine
Doctors don’t jump straight to Clozapine. They usually try other antipsychotics first. These are the most common alternatives:
- Olanzapine - Similar in structure to Clozapine, it’s often used as a stepping stone. It’s effective for positive symptoms like hallucinations but carries higher risk of weight gain and metabolic issues.
- Risperidone - Works well for acute psychosis and is easier to manage. It has fewer blood monitoring requirements, but can cause muscle stiffness and elevated prolactin levels.
- Quetiapine - Popular for its sedating effect. Often used when sleep problems are part of the illness. Less risk of movement disorders, but still linked to weight gain and high cholesterol.
- Aripiprazole - A partial dopamine agonist. It’s less likely to cause weight gain or sedation, but can trigger restlessness and anxiety in some.
- Paliperidone - The active metabolite of risperidone, available as a monthly injection. Good for people who struggle with daily pills.
None of these match Clozapine’s effectiveness in treatment-resistant cases. But they’re safer, easier to monitor, and often tried first.
Comparing Effectiveness and Side Effects
Choosing between Clozapine and alternatives isn’t just about which drug works better. It’s about what you can live with long-term.
| Drug | Effectiveness in Treatment-Resistant Cases | Major Side Effects | Monitoring Required | Form |
|---|---|---|---|---|
| Clozapine | Best - 40-60% response rate | Agranulocytosis, seizures, weight gain, constipation, heart issues | Weekly blood tests (first 6 months), then biweekly | Oral tablet or orally disintegrating tablet |
| Olanzapine | Moderate - 25-35% response | Weight gain, high blood sugar, high cholesterol | None beyond routine checkups | Oral tablet, injectable |
| Risperidone | Moderate - 20-30% response | Muscle stiffness, tremors, elevated prolactin, sexual side effects | None beyond routine checkups | Oral tablet, liquid, long-acting injection |
| Quetiapine | Moderate - 20-30% response | Drowsiness, weight gain, dizziness, dry mouth | None beyond routine checkups | Oral tablet, extended-release |
| Aripiprazole | Mild to moderate - 15-25% response | Restlessness, nausea, insomnia, akathisia | None beyond routine checkups | Oral tablet, long-acting injection |
Looking at this table, the pattern is clear: Clozapine wins on effectiveness but loses on safety and convenience. The alternatives are easier to manage but often fall short when symptoms are severe and stubborn.
Who Should Consider Clozapine?
Not everyone with schizophrenia needs Clozapine. But if you’ve tried at least two antipsychotics - each for at least six weeks at adequate doses - and still hear voices, believe things that aren’t true, or feel completely disconnected from reality, Clozapine may be your best shot.
It’s also the only antipsychotic proven to reduce suicide risk in schizophrenia. For people with a history of self-harm or suicidal thoughts, this alone can make it the top choice.
But if you have:
- History of low white blood cell counts
- Severe heart problems
- Uncontrolled epilepsy
- Difficulty keeping up with weekly blood tests
Then Clozapine is likely too risky. Your doctor may recommend long-acting injections like paliperidone or risperidone instead.
What If Clozapine Doesn’t Work?
Even Clozapine fails in about 30-40% of treatment-resistant cases. When that happens, options are limited. Some doctors add mood stabilizers like lithium or valproate. Others try combining antipsychotics - though this is controversial and not recommended by most guidelines.
There’s also emerging research on non-drug treatments. Repetitive transcranial magnetic stimulation (rTMS) has shown promise in reducing auditory hallucinations. Cognitive behavioral therapy for psychosis (CBTp) helps people manage symptoms even when medication doesn’t fully eliminate them. These aren’t replacements for medication, but they can make life more manageable.
For a small group, electroconvulsive therapy (ECT) is still used - especially when symptoms are severe and life-threatening. It’s not common, but it works for some who’ve tried everything else.
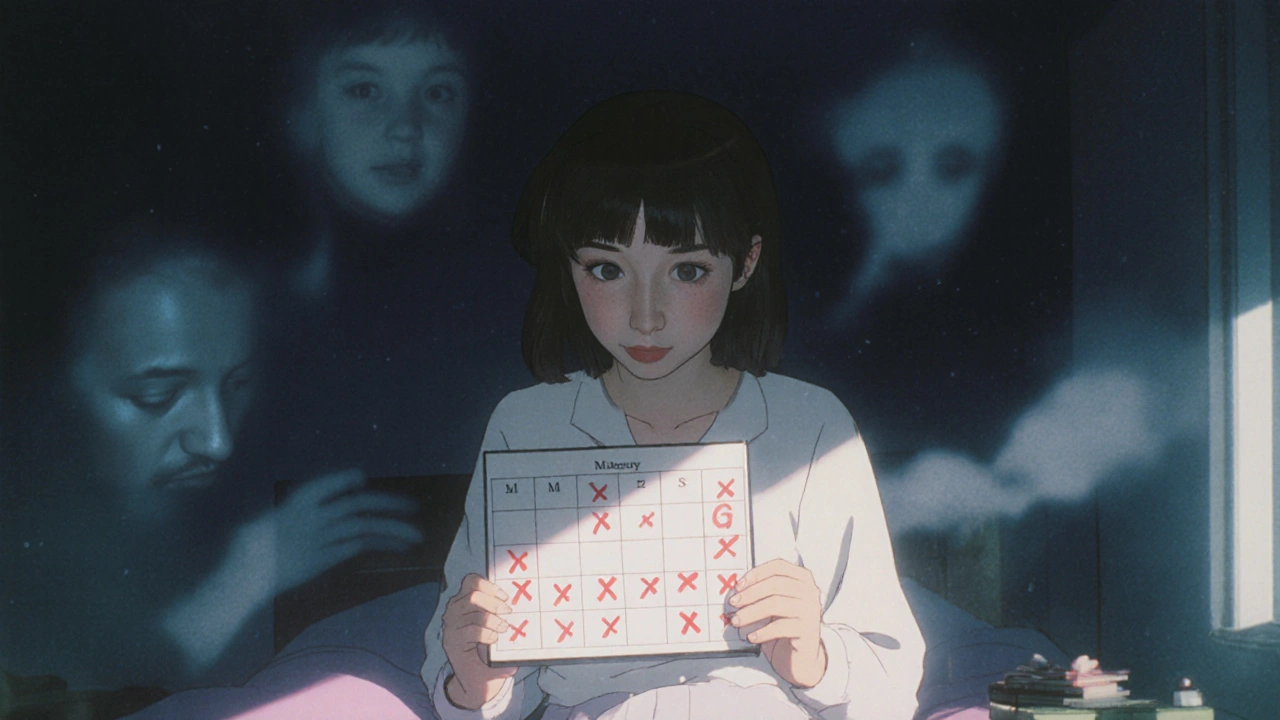
Real-Life Trade-Offs
One patient I worked with in Halifax - let’s call her Sarah - tried seven antipsychotics over seven years. Each one made her feel worse: too sleepy, too heavy, too jittery. Her hallucinations didn’t stop. She stopped leaving her house. Her family was exhausted.
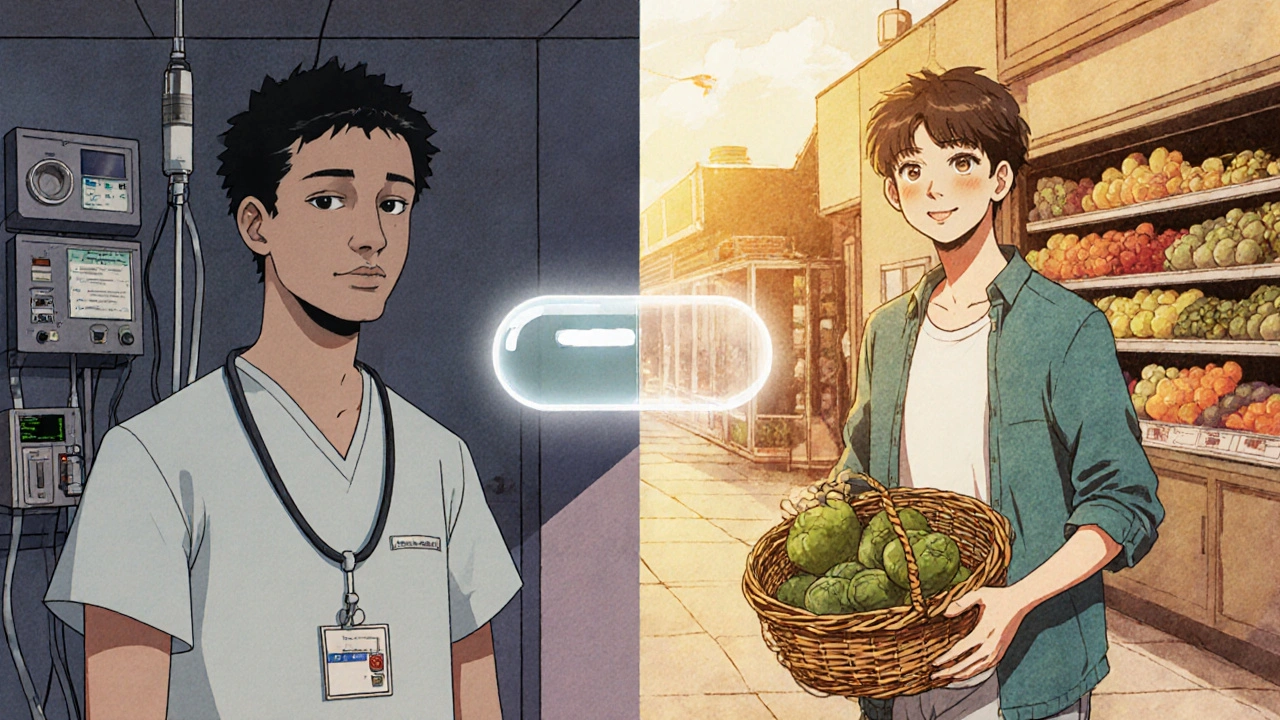
When she started Clozapine, her white blood cell count dropped the first month. She had to go to the clinic every week. She missed work. She was scared. But after three months, she started laughing again. She went to the grocery store. She called her sister. That’s the kind of change Clozapine can bring - if you can survive the process.
On the other side, a man in his 50s tried Clozapine but couldn’t handle the blood tests. He lived alone, had no family nearby, and forgot appointments. His symptoms returned. His doctor switched him to a monthly risperidone injection. It wasn’t as effective, but it kept him stable enough to live independently.
There’s no universal answer. What works for one person might be a disaster for another.
When to Ask for a Second Opinion
If your doctor hasn’t mentioned Clozapine after you’ve tried two or more antipsychotics, ask why. Not every psychiatrist is comfortable prescribing it. Some avoid it because of the monitoring burden. Others don’t know the latest guidelines.
Don’t be afraid to seek a specialist - a psychiatrist who focuses on treatment-resistant psychosis. They’re more likely to know when Clozapine is the right move, and how to make the process manageable.
Also, ask about patient support programs. Many hospitals and pharmacies offer free blood testing, transportation help, and nurse check-ins. You don’t have to do this alone.
Final Thoughts
Clozapine isn’t a miracle drug. It’s a powerful, risky tool - one that can restore someone’s life or take it away if mismanaged. The alternatives are safer, but often less effective. The choice isn’t between good and bad. It’s between different kinds of risk.
If you’re considering Clozapine, make sure you understand the blood tests, the side effects, and the long-term commitment. If you’re choosing an alternative, know that you might need to try more than one before finding something that sticks.
There’s no rush. Schizophrenia treatment isn’t a sprint. It’s a long walk with many turns. The goal isn’t perfection - it’s enough stability to live, to connect, to hope.
Is Clozapine the most effective antipsychotic for treatment-resistant schizophrenia?
Yes. Clozapine is the only antipsychotic proven to work better than others in people who haven’t responded to at least two other drugs. Studies show it helps 40-60% of treatment-resistant cases, compared to under 30% for alternatives like olanzapine or risperidone. It’s also the only one shown to reduce suicide risk in this group.
Why is Clozapine not used as a first-line treatment?
Because of its serious side effect - agranulocytosis, which can cause life-threatening infections. To prevent this, patients must get weekly blood tests for the first six months, then every two weeks after. Many doctors avoid prescribing it unless absolutely necessary because of the monitoring burden and risk.
Can you switch from Clozapine to another antipsychotic safely?
Yes, but it must be done carefully. Stopping Clozapine suddenly can cause rebound psychosis or severe withdrawal symptoms like nausea, vomiting, and insomnia. Doctors usually taper the dose slowly over weeks or months and start the new drug at a low dose while gradually reducing Clozapine. Close monitoring is essential during this transition.
What are the biggest side effects of Clozapine?
The most dangerous is agranulocytosis - a drop in white blood cells. Other major side effects include seizures (especially at higher doses), weight gain, constipation (which can become life-threatening), increased heart rate, and drooling. Some people also develop myocarditis, an inflammation of the heart muscle, especially in the first few months.
How long does it take for Clozapine to work?
Improvement can start in 2-4 weeks, but full effects often take 3-6 months. Many patients don’t see major changes until after the third month. Patience is key. If there’s no sign of improvement by six months, the drug is unlikely to work for that person.
Are there any new alternatives to Clozapine on the horizon?
There’s no new drug yet that matches Clozapine’s effectiveness. Researchers are testing drugs like pimavanserin and lumateperone, but none have shown the same level of success in treatment-resistant cases. Some are exploring combination therapies or using genetic testing to predict who might respond better to certain drugs. For now, Clozapine remains the gold standard - despite its risks.
If you’re managing treatment-resistant schizophrenia, you’re not alone. The path is hard, but options exist. The key is working with a team that understands both the science and the human cost of each choice.





12 Comments
Clozapine saved my brother's life, but man, those blood tests were a nightmare. He missed one once because of a snowstorm and had to stop cold turkey. Came back worse than before. We were terrified.
Now he's on monthly injections and it's not perfect, but he's laughing again. That's all we ever wanted.
They say clozapine is the only thing that works but i think the pharma companies just want you hooked on the most expensive drug so they can charge more for the blood tests and the monitoring and the special pills and the nurses and the follow ups and the paperwork and the forms and the waiting and the stress and the fear and the guilt and the shame and the loss of dignity and the loss of control and the loss of your damn life
Let me guess - you’re one of those people who thinks ‘40-60% response rate’ means it’s a miracle cure. Newsflash: that’s still nearly half the people who don’t improve. And you’re glorifying a drug that turns people into drooling, obese zombies with heart issues and seizures. What’s next, recommending insulin for weight loss?
I’m a nurse who’s seen this play out a hundred times. The fear around clozapine is real, but so is the stigma. I’ve had patients cry because their doctor refused to even discuss it. They think it’s too risky - but not risking it is riskier. The suicide reduction data is undeniable. If you’ve tried everything else, this isn’t a last resort. It’s the next step.
My cousin tried clozapine and it worked - for a while. Then he got constipation so bad he ended up in the ER. No one warned him how bad that could get. They focus on the blood tests, but the GI stuff? Barely mentioned. He’s on olanzapine now and it’s not as good, but at least he can eat without pain. I wish the docs talked more about the whole picture, not just the headline stats.
I was on clozapine for 18 months. I lost 40 pounds because I couldn’t eat. My mouth was dry all day, I drooled like a baby, and I had nightmares so vivid I thought I was still hallucinating. But… I heard my mom’s voice for the first time in 5 years. She said ‘I love you.’ I haven’t cried like that since I was 12. So yeah, it broke me. But it also rebuilt me. I’d do it again.
So clozapine = miracle. Alternatives = trash. Got it. 😒
Let’s be real - clozapine is the nuclear option. It’s not medicine, it’s a psychological Hail Mary. The system doesn’t want you to have it. Too much responsibility. Too much liability. Too many people asking too many questions. So they shove you into risperidone injections and call it a day. Meanwhile, the ones who could’ve been whole? Left in the shadows. This isn’t science. It’s risk-aversion dressed up as protocol.
My cousin in Cork was on clozapine. They did the blood tests every week like clockwork. He got a free bus pass for clinic trips. The hospital even had a nurse call him every morning to remind him. It wasn’t perfect - he gained weight, slept all day - but he held a job for two years. That’s more than he’d done in a decade. If we can make this manageable, why don’t we do it more often?
Look, I get why people are scared of clozapine. But here’s the thing - the alternatives aren’t safe. They’re just quieter. Olanzapine makes you fat and diabetic. Risperidone turns you into a robot with no libido. Aripiprazole gives you restless legs and anxiety attacks. Clozapine? It’s loud, it’s messy, it’s brutal - but it doesn’t just numb you. It lets you come back. If you’ve got the support system? It’s worth it. If you don’t? Then the system failed you, not the drug.
Why do we keep pretending this is a medical decision? It’s a logistical one. Who’s going to drive you to the lab every week? Who’s going to remember? Who’s going to pay for the time off work? Who’s going to sit with you when you’re scared? If the answer is ‘no one,’ then clozapine isn’t an option - it’s a trap. And we’re selling it like it’s a gift.
In Japan, they use clozapine more liberally - but with a structured community care model. Nurses visit homes, pharmacies deliver blood kits, and patients are never alone. Why don’t we adopt that here? It’s not about the drug. It’s about the care infrastructure. Without it, clozapine is just another burden. With it? It’s a lifeline.