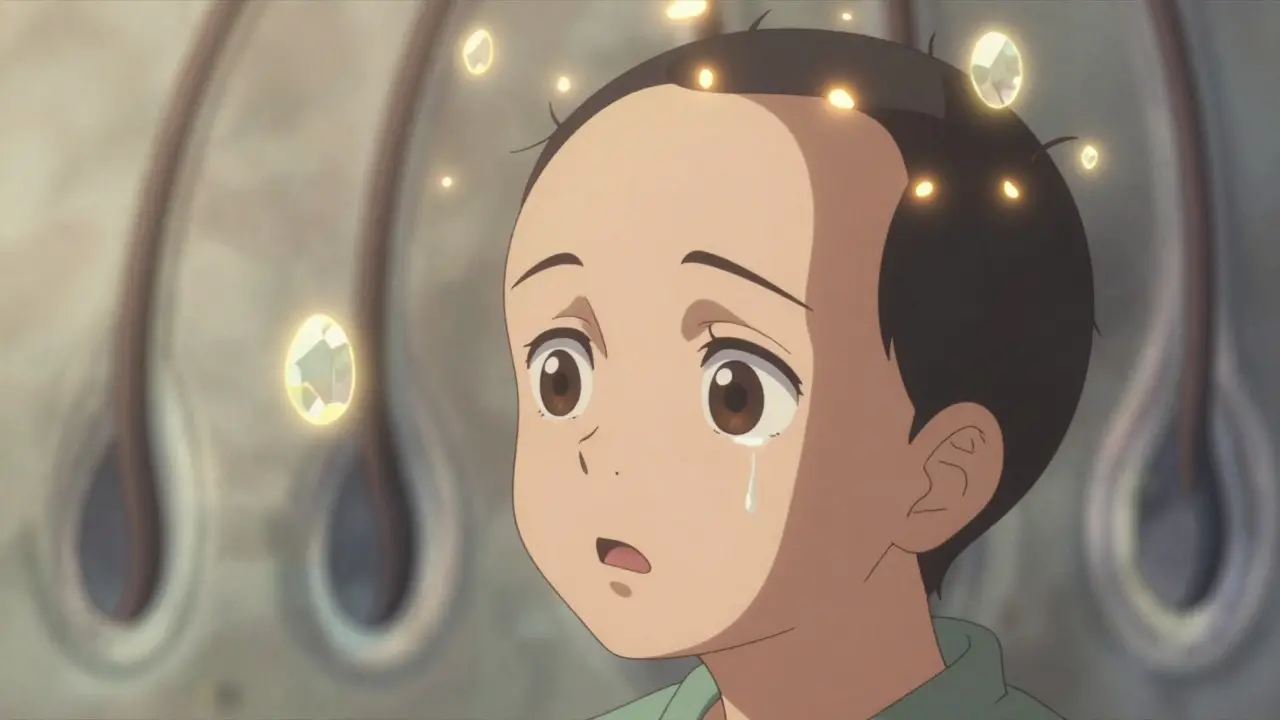
Alopecia areata isn’t just about losing hair-it’s about your immune system turning against your own hair follicles. Unlike male or female pattern baldness, which happens slowly over years, alopecia areata strikes suddenly. One day you have a full head of hair; the next, you notice a smooth, round patch-about the size of a quarter-where hair used to be. It doesn’t hurt. It doesn’t itch, at first. But the shock? That’s real. And it’s more common than most people think.
Around 6.8 million people in the U.S. will experience alopecia areata in their lifetime. Globally, it affects 0.1% to 0.2% of the population. It doesn’t care if you’re 5 or 50. Half of all cases start before age 40, and men and women are equally likely to get it. What sets it apart is that your hair follicles aren’t destroyed. They’re put into hibernation. That’s why regrowth is possible-even after years of total baldness.
How Your Immune System Attacks Your Hair
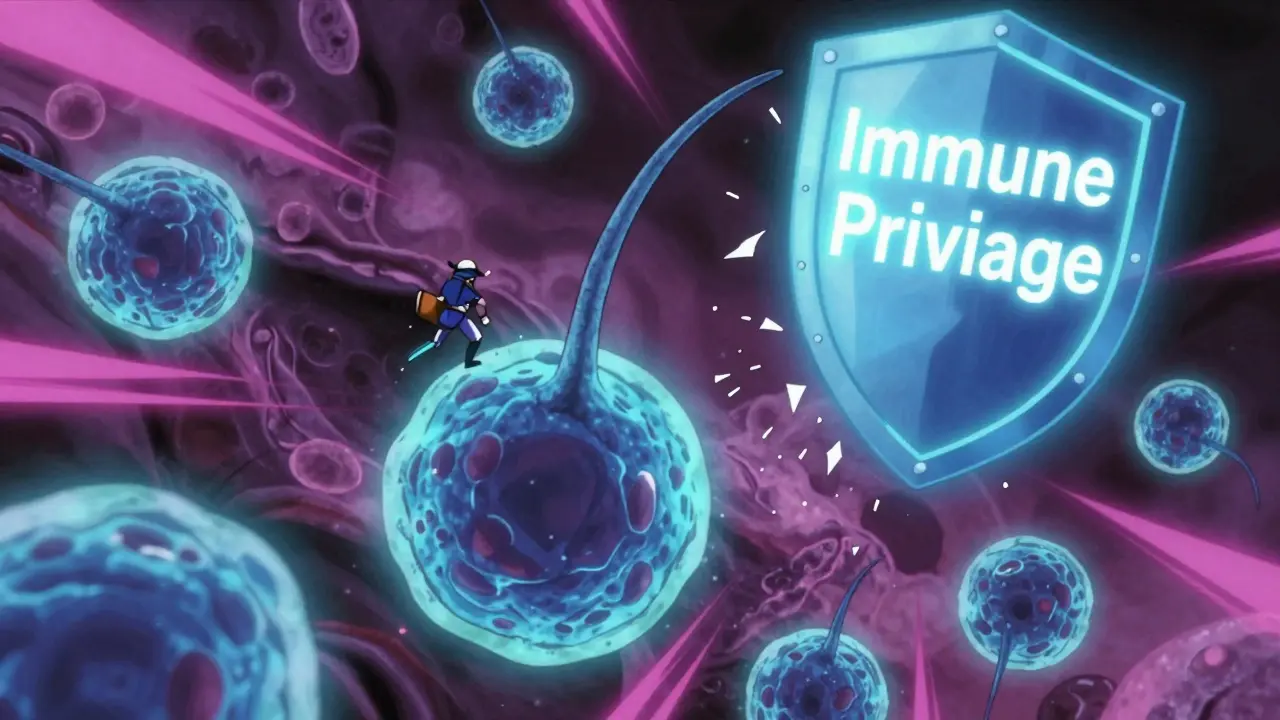
Your hair grows in cycles: active growth (anagen), transition (catagen), and rest (telogen). Normally, hair follicles are protected by something called "immune privilege." Think of it like a quiet zone where immune cells aren’t allowed to bother the follicle. In alopecia areata, that protection breaks down. Immune cells-mainly CD8+ T cells and natural killer cells-cluster around the base of the follicle like an angry swarm. They don’t kill the follicle. They just force it to stop growing and enter the resting phase too early.
This is why the bald patches look so smooth. No scarring. No inflammation. Just empty space where hair used to be. The follicles are still alive. They’re just on pause. That’s also why some people regrow hair spontaneously-even after losing all of it. About 80% of people with small patches see regrowth within a year without any treatment.
The Different Faces of Alopecia Areata
Alopecia areata doesn’t show up the same way for everyone. There are several forms:
- Patchy alopecia areata: One or more coin-sized bald spots on the scalp. This is the most common type.
- Alopecia totalis: Complete loss of all scalp hair.
- Alopecia universalis: Total loss of all body hair-including eyebrows, eyelashes, armpits, and pubic hair.
- Diffuse alopecia areata: Sudden thinning across the whole scalp, mimicking general hair shedding.
- Ophiasis: Hair loss in a band-like pattern around the sides and back of the head.
Some people also notice changes in their nails. About 1 in 3 patients develop tiny dents (pitting), rough surfaces (trachyonychia), or redness near the nail base. These signs can appear before hair loss even starts.
What Triggers It?
No one knows exactly what starts the immune system’s attack. Genetics play a role-if you have a close relative with alopecia areata, your risk is higher. But genes alone don’t cause it. Environmental triggers seem to be needed. Stress is often blamed, but it’s not the root cause. More likely, it’s a combination of factors: viral infections, hormonal shifts, or even certain chemicals that confuse the immune system.
Research has found specific genes linked to the condition, like ULBP3 and ULBP6. These genes help immune cells recognize hair follicles as targets. That’s why scientists are now working on tests to predict who’s most likely to develop severe forms-and who might respond best to certain treatments.
Treatment Options: What Actually Works
There’s no cure. But there are treatments that can help hair grow back-sometimes fully. The effectiveness depends on how much hair you’ve lost and how long it’s been gone.
Intralesional Corticosteroid Injections
This is the go-to first-line treatment for patchy alopecia. A dermatologist injects a diluted steroid (usually triamcinolone acetonide) directly into each bald patch every 4 to 6 weeks. It works by calming the immune attack right where it’s happening.
Success rate? Around 60% to 67% of people with small patches see regrowth within 3 to 6 months. It’s fast, targeted, and relatively safe. But it doesn’t work for large areas or total hair loss. And it hurts-like a bee sting. Multiple injections are needed, so it’s not for everyone.
Topical Steroids and Minoxidil
For milder cases, doctors sometimes prescribe steroid lotions or foams (like 0.1% betamethasone valerate). These are applied daily. But results take 6 to 12 months-and only about 25% to 30% of people see noticeable regrowth.
Minoxidil (Rogaine) is often added on top. It’s not an immune modulator. It just stimulates hair growth. For patchy alopecia, it helps maybe 10% to 15% of people. For total or universal hair loss? Almost no effect. Still, many use it because it’s over-the-counter and low-risk.
Contact Immunotherapy (DPCP)
This is a strange but effective option for people with extensive hair loss. You apply a chemical called diphenylcyclopropenone (DPCP) to your scalp weekly. It doesn’t grow hair-it causes a mild allergic reaction. That reaction tricks your immune system into ignoring the hair follicles.
It takes 6 to 12 months to work. Side effects include redness, blistering, and itching. But for those who stick with it, 30% to 60% see significant regrowth. It’s not widely available because it requires special training to use safely.
JAK Inhibitors: The New Game Changer
In 2022, the FDA approved baricitinib (Olumiant) for severe alopecia areata. It was the first oral drug ever approved specifically for this condition. It works by blocking JAK enzymes-key players in the immune signal that attacks hair follicles.
In clinical trials, 35.6% of patients with severe alopecia areata got back 80% or more of their scalp hair after 36 weeks. That’s huge. Another drug, ritlecitinib, got FDA approval in June 2023, with similar results.
But there’s a catch. These drugs cost $10,000 to $15,000 per month. Insurance often denies coverage. And they’re not permanent fixes. About 75% of people lose their hair again within a year of stopping the medication. Still, for many, it’s the first real hope they’ve had.
Why Some Treatments Fail
Not everyone responds. And no treatment works for everyone. Why?
- Extent of loss: Treatments that work for small patches rarely help with total hair loss.
- Duration: The longer hair has been gone, the harder it is to regrow.
- Age: Children often respond better than adults.
- Genetics: Some people’s immune systems just don’t respond to the drugs.
Many patients try multiple treatments over years. One Reddit user shared: "I did 18 steroid injections over two years. Got a little regrowth, then lost it again. Felt like I was paying for false hope."

The Emotional Toll
Alopecia areata doesn’t kill you. But it can break you.
Studies show 30% of patients have moderate to severe anxiety. 28% meet the criteria for clinical depression. In a 2022 survey by the National Alopecia Areata Foundation, 68% of respondents said they avoided social situations because of their appearance. 42% stopped going to the beach or swimming pools.
It’s not vanity. It’s identity. Hair is tied to how we see ourselves-and how others see us. Losing it suddenly can feel like losing a part of your body. That’s why support groups, counseling, and even wigs or scalp micropigmentation matter as much as medical treatment.
What’s Next?
Research is moving fast. Scientists at Columbia University are developing blood tests to predict who will respond to JAK inhibitors. Others are testing combination therapies-like pairing a JAK inhibitor with low-dose steroids or light therapy-to reduce relapse rates.
The National Institutes of Health spent $12.7 million on alopecia areata research in 2023-a 23% increase from 2020. Four new JAK inhibitors are in late-stage trials. One goal: treatments that reset the immune system instead of just suppressing it.
By 2030, the National Alopecia Areata Foundation believes they can cut the disease’s impact by half. That means fewer people living in fear, fewer skipped weddings, fewer kids bullied at school.
For now, the message is this: you’re not alone. Regrowth is possible. Even if it takes years. Even if it comes back gray at first. Even if it falls out again. The science is catching up. And your worth isn’t tied to your hair.
Frequently Asked Questions
Can alopecia areata be cured?
There is no permanent cure yet. Current treatments can help hair regrow, but they don’t fix the underlying immune issue. Most people experience relapses, especially after stopping medication. Researchers are working on therapies that could reset the immune system, but those are still in development.
Does stress cause alopecia areata?
Stress doesn’t cause alopecia areata, but it can trigger flare-ups in people who are genetically predisposed. The root cause is autoimmune dysfunction-not emotional stress. However, the stress of living with hair loss can make the condition worse, creating a cycle that’s hard to break.
Will my hair grow back if I lose all of it?
It’s possible, but unlikely. About 10% of people with alopecia universalis (total body hair loss) regain full hair permanently without treatment. With treatment, especially JAK inhibitors, some see significant regrowth. But most will experience cycles of loss and regrowth over time.
Are JAK inhibitors safe for long-term use?
JAK inhibitors like baricitinib and ritlecitinib are FDA-approved for severe alopecia areata, but they carry risks. These include increased chances of infection, blood clots, and certain cancers. They’re typically reserved for patients with extensive hair loss who haven’t responded to other treatments. Regular blood tests and doctor monitoring are required.
Can children get alopecia areata?
Yes. About half of all cases begin before age 40, and many start in childhood. Children often respond better to treatment than adults. Intralesional steroids and topical therapies are commonly used. Emotional support is especially important-bullying and self-esteem issues are common in school-aged kids with visible hair loss.
Is alopecia areata the same as telogen effluvium?
No. Telogen effluvium causes diffuse thinning across the scalp due to stress, illness, or nutritional changes. It’s temporary and doesn’t create distinct bald patches. Alopecia areata is autoimmune, causes patchy loss, and can persist for years. The treatments are completely different.
Can I use natural remedies like essential oils or supplements?
There’s no strong scientific evidence that essential oils, coconut oil, or supplements like biotin reverse alopecia areata. Some people report mild improvement, but it’s likely due to placebo or coincidental regrowth. These won’t stop the immune attack. If you’re considering them, talk to your dermatologist first-some oils can irritate the scalp and make things worse.
How do I know if I have alopecia areata and not something else?
A dermatologist can usually diagnose it by looking at the bald patches-smooth, round, no scaling or scarring. They may do a pull test (gently tugging on hairs) or examine hair under a microscope. In unclear cases, a small skin biopsy can confirm the immune cells clustering around follicles. Don’t rely on online photos-other conditions like fungal infections or lupus can look similar.





12 Comments
lol so basically your immune system got a bad case of mistaken identity and decided to cancel your hair follicles. cool. now how do i get my insurance to pay for this?
I lost my hair at 22. Thought I was broken. Turned out I was just a human with a misfiring defense system. The regrowth came slow, gray, patchy - but it came. You’re not your hair. You’re the person who kept showing up anyway. 🌱
I remember sitting in a dermatologist’s office in London, staring at the bald spot on my scalp like it was a foreign planet. The doctor said, ‘It’s not cancer, it’s not contagious, it’s just… your body being weird.’ And that’s when I started to breathe again. Hair grows back. People change. But your worth? That’s always been yours. No vaccine needed.
The FDA approval of JAK inhibitors is statistically significant but clinically questionable. Relapse rates exceed 75% post-treatment cessation. Cost-benefit analysis demonstrates marginal utility for public health expenditure given the low prevalence. Long-term safety profiles remain inadequately characterized.
I’ve been through three rounds of steroid shots. Felt like a pin cushion. But when I saw that one little strand grow back? I cried. Not because I wanted to look ‘normal’ - but because I finally felt like my body wasn’t trying to kill me. You’re not alone. 💪❤️
My cousin lost all her eyebrows. Now she draws them on with eyeliner like a warrior. She won a beauty pageant last year. No hair. No problem.
This is all a cover-up. The real cause is 5G radiation and GMO soy. The pharmaceutical companies profit from your fear. They don’t want you to know about the ancient Indian herb that cures everything. Google 'Kutki root' and wake up.
I’m a dad with patchy alopecia. My 7-year-old asked me if I was a superhero because my head was shiny. I said yes. Now he calls me ‘Captain Smooth’. Sometimes the bravest thing you can do is let your kid see you unapologetically you. 🦸♂️
Minoxidil doesn’t fix the immune issue. But if it helps you feel less anxious while waiting for better treatments? Worth a shot. Low risk, zero shame.
The immune privilege hypothesis is fascinating - follicles are immunologically privileged sites due to low MHC-I expression, and the breakdown of this barrier via ULBP3/6 upregulation triggers CD8+ T-cell infiltration. JAK inhibition disrupts the IFN-γ/STAT1 axis, which is central to the pathogenic cascade. Still, the psychosocial burden remains grossly under-addressed in clinical trials.
The government spends millions on this because they don't want Americans to look different. Uniformity is national security. Hair is a symbol of loyalty. You think this is medicine? It's control.
I had alopecia at 16. Tried everything. Gave up. Then one day, my beard grew back first. Then my eyebrows. Now my scalp? 80% full. Took 5 years. No magic. Just patience. You got this.