Most people know that high blood pressure can hurt your heart or kidneys. But few realize it’s also quietly damaging the tiny blood vessels in your eyes-sometimes long before you notice any vision problems. Hypertensive retinopathy isn’t a sudden event. It’s a slow, silent breakdown of your retina’s blood supply, caused by years of uncontrolled hypertension. And by the time you see blurry vision or dark spots, the damage may already be serious-or even permanent.
What Exactly Is Hypertensive Retinopathy?
Hypertensive retinopathy happens when high blood pressure forces your retinal arteries to work too hard. Over time, their walls thicken and narrow, cutting off oxygen and nutrients to the light-sensitive tissue at the back of your eye. This isn’t just about pressure on the vessels-it’s about leakage, blockage, and tissue death.
The changes don’t happen overnight. Studies show that after just 3-5 years of uncontrolled blood pressure above 140/90 mmHg, early signs like narrowed arteries start appearing. By year 10, even "mild" hypertension (130-139 mmHg systolic) can cause visible damage. The retina becomes a mirror for your overall vascular health. What’s happening in your eyes often reflects what’s happening in your brain, heart, and kidneys.
How Doctors Grade the Damage
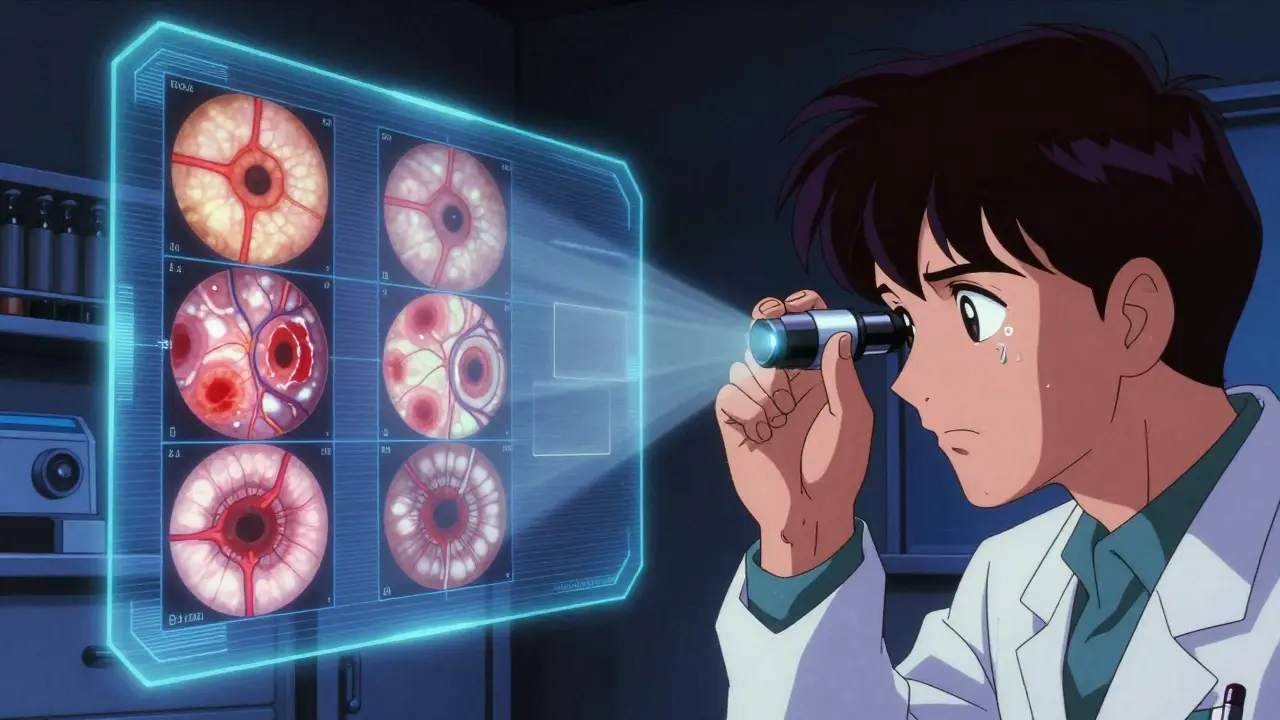
Doctors use the Keith-Wagener-Barker (KWB) system to classify how far the damage has gone. It’s not just a label-it tells you how urgent your situation is.
- Grade 1: Barely noticeable. Arteries are slightly narrower. No bleeding or swelling. Most people feel nothing.
- Grade 2: Arteries are more constricted, and you’ll see "nicking"-where a vein gets pinched where it crosses an artery. This is a red flag. About 22% of people with stage 1 hypertension show this after 3 years.
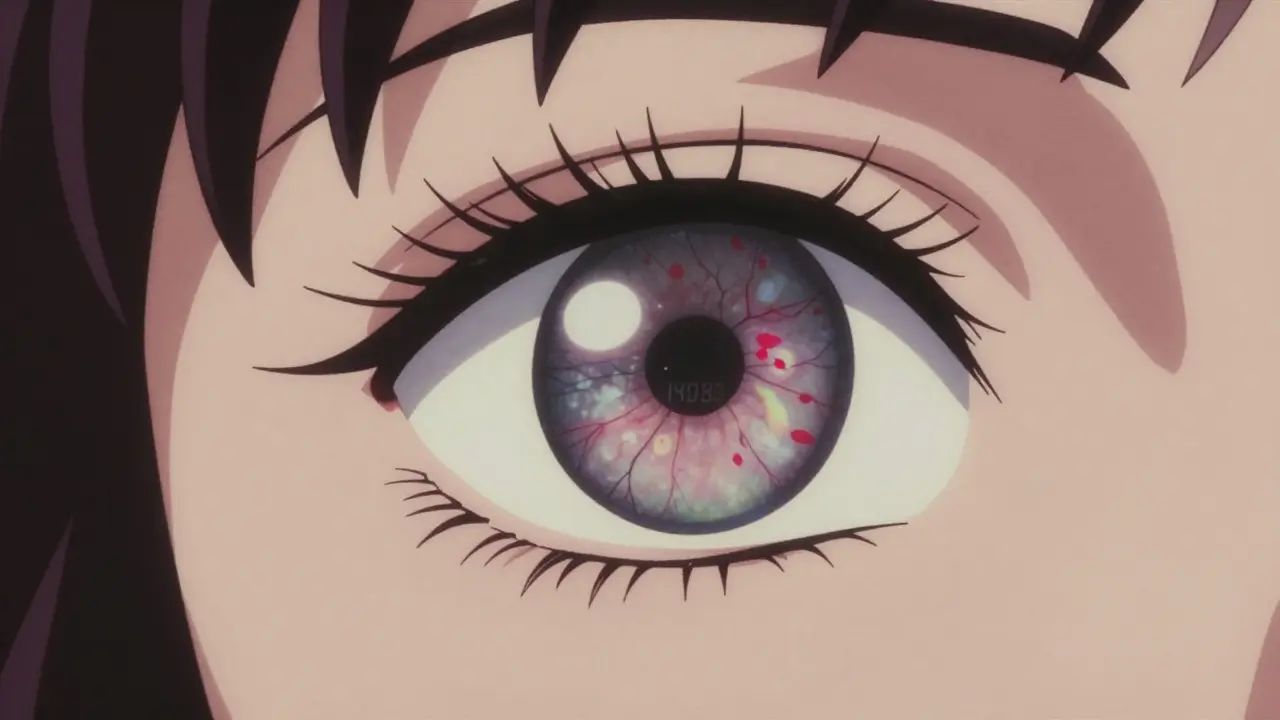
- Grade 3: Now you’ve got hemorrhages (tiny bursts of blood), cotton wool spots (white patches from nerve damage), and hard exudates (fatty leaks). Vision may start to blur. This stage means your blood pressure is dangerously high and has been for a while.
- Grade 4: The worst. All of the above, plus swelling of the optic nerve (papilledema). This is malignant hypertension. It’s a medical emergency. Patients at this stage have a 78% higher risk of stroke and often have kidney or heart failure too.
Retinal imaging tools like optical coherence tomography (OCT) can measure how much the retina has thickened-up to 15% in advanced cases. These aren’t just pictures. They’re warning signs your body is screaming for help.
Why You Might Not Notice Anything-Until It’s Too Late
Here’s the scary part: 68% of people with early-stage hypertensive retinopathy (Grades 1-2) have no symptoms at all. No pain. No blurriness. No floaters. You could be walking around with damaged retinal vessels and feel fine.
By the time symptoms appear, you’re likely already in Grade 3 or 4. That’s when you might see:
- Blurred or dim vision
- Sudden dark spots or blind spots in your central vision
- Double vision with headaches
- A "curtain" falling over part of your visual field
One Reddit user described waking up with dark spots after his blood pressure spiked to 210/110. Another reported double vision and crushing headaches-classic signs of a hypertensive emergency. But most patients don’t connect these symptoms to their blood pressure. Clinical data shows 42% wait 18-24 months before seeking help, assuming it’s just aging or eye strain.
What Happens If You Ignore It?
Ignoring hypertensive retinopathy isn’t just risking your vision. It’s risking your life.
Retinal changes are strong predictors of bigger problems:
- Patients with arteriovenous nicking have a 3.2x higher risk of stroke.
- Those with optic nerve swelling are far more likely to have heart failure or kidney disease.
- Even mild retinopathy doubles your risk of heart attack or stroke within 5 years.
And once the retina is damaged-especially the macula, where sharp vision happens-recovery is limited. Some people regain partial sight after lowering their blood pressure, but 22% end up with permanent visual field loss. The longer the pressure stays high, the less chance there is for full recovery.
How to Catch It Early
The best way to stop this before it starts? Routine eye exams.
Eye doctors can spot Grade 1 changes during a simple fundoscopic exam-even if your blood pressure is only 140/90. That’s why the American Academy of Ophthalmology recommends annual eye checks for anyone with hypertension. If your blood pressure is uncontrolled or you have resistant hypertension (still high despite three medications), they now recommend exams every 6 months.
Technology is helping too. AI tools like RetinaCheck AI and IDx-DR can analyze retinal images with 92% accuracy-up from 75% just a few years ago. These systems are now being used in primary care clinics, not just eye specialists. If your doctor has a digital retinal camera, ask if they’ve checked your eyes for signs of hypertension damage.
Can You Reverse the Damage?
Yes-but only if you act fast.
Lowering your systolic blood pressure by 25 mmHg within 48 hours can reverse early retinal changes in 65% of cases. That means bringing a reading of 180/110 down to around 155/90 quickly. But you can’t do this by yourself. If your blood pressure is over 180/120, you need urgent medical care-not just a pill.
Medication matters. A 2023 study found ACE inhibitors reduce retinal damage progression by 32% more than calcium channel blockers. That’s not a small difference. It’s life-changing for your eyes.
For stable patients with Grade 1-2 retinopathy, annual checkups and consistent medication use are enough. But if you’re at Grade 3 or higher, you need:
- Immediate blood pressure control
- Regular ophthalmology visits
- Monitoring for kidney and heart issues
Recovery takes time. Vision improvement usually starts in 7-10 days, but full healing can take 3-6 months. And if the macula is damaged, you may never get back 100% of your vision.

What You Can Do Today
If you have high blood pressure, here’s your action plan:
- Know your numbers. Check your blood pressure at home. Don’t rely on one reading at the doctor’s office. Take readings twice a day for two weeks and track them.
- Get your eyes checked. If you haven’t had a dilated eye exam in the last year, schedule one. Don’t wait for symptoms.
- Treat it like a system-wide problem. Your eyes aren’t isolated. What’s hurting them is hurting your heart, brain, and kidneys. Medication, diet, exercise, and stress control all matter.
- Don’t ignore warning signs. Blurry vision, sudden dark spots, or headaches with high BP? Go to the ER or call your doctor immediately.
There’s good news: 85% of early-stage cases stabilize with proper blood pressure control. You’re not doomed. But you have to act.
Special Risks for Diabetics
If you have both diabetes and high blood pressure, your risk of vision loss jumps dramatically. The American Diabetes Association says you’re 4.7 times more likely to suffer permanent damage from combined retinopathies. That’s not a coincidence. Diabetes and hypertension both attack small blood vessels. Together, they’re a perfect storm for blindness.
If you’re diabetic and hypertensive, don’t wait for your annual eye exam. Get checked every 6 months. Ask your doctor about ACE inhibitors-they’re especially protective in this group.
The Bigger Picture
Hypertensive retinopathy affects nearly 20 million Americans. That’s 7.3% of the adult population. And it’s growing. The diagnostic market for this condition is projected to hit $1.8 billion by 2027 as more clinics adopt AI imaging.
But numbers don’t tell the real story. The real story is the person who ignored their blood pressure for years, then woke up with vision loss. The one who didn’t connect their blurry sight to their hypertension meds. The one who thought "I feel fine," so everything must be okay.
Your eyes don’t lie. They show you what your blood pressure is doing to your body-long before you feel it. If you have high blood pressure, your eyes are your early warning system. Don’t wait for the alarm to scream before you listen.
Can hypertensive retinopathy cause blindness?
Yes, if left untreated. Advanced stages (Grade 3-4) can lead to permanent vision loss, especially if the macula or optic nerve is damaged. While early detection and blood pressure control can prevent or reverse damage, delays in treatment increase the risk of irreversible vision impairment.
Does high blood pressure always damage the eyes?
No-not everyone with high blood pressure develops retinopathy. But the longer your blood pressure stays elevated and the higher it goes, the greater the risk. About 22% of people with stage 1 hypertension show signs after 3 years. Nearly half of those with stage 2 hypertension will develop visible retinal changes within 5 years.
Can lifestyle changes reverse hypertensive retinopathy?
Lifestyle changes alone usually aren’t enough to reverse advanced damage, but they’re critical for stopping progression. Reducing salt, losing weight, exercising, and limiting alcohol can lower blood pressure enough to stabilize the retina. For early-stage cases, combining lifestyle changes with medication often leads to improvement. But if you’re already at Grade 3 or higher, medication is essential.
How often should I get my eyes checked if I have high blood pressure?
If your blood pressure is controlled and you have no retinal changes, an annual eye exam is enough. If you have Grade 1-2 retinopathy, stick with yearly checks. If your blood pressure is uncontrolled or you have resistant hypertension (still high after three medications), get checked every 6 months. If you’re diabetic and hypertensive, every 6 months is mandatory.
Is hypertensive retinopathy the same as diabetic retinopathy?
No. They’re different conditions, but they often occur together and both damage retinal blood vessels. Diabetic retinopathy is caused by high blood sugar, while hypertensive retinopathy is caused by high blood pressure. The damage looks similar-bleeding, leakage, swelling-but the root causes and treatment approaches differ. Having both dramatically increases your risk of blindness.
Can I check for hypertensive retinopathy at home?
No. You cannot detect retinal damage at home. While home blood pressure monitors help track your numbers, they don’t show eye damage. Only an eye doctor using a fundoscope or retinal camera can spot the early signs like narrowed arteries, hemorrhages, or optic nerve swelling. Don’t rely on vision apps or phone cameras-they’re not accurate enough.
What’s the most dangerous sign of hypertensive retinopathy?
Papilledema-swelling of the optic nerve-is the most dangerous sign. It indicates malignant hypertension, a life-threatening condition. It often comes with sudden vision loss, severe headaches, and confusion. If you have this, you need emergency treatment. Delaying care can lead to stroke, heart attack, or permanent blindness within hours.


10 Comments
Everyone talks about blood pressure like it’s some newfangled problem, but this has been staring us in the face since the 1950s. We’ve got a whole generation raised on processed food, soda, and zero movement. The retina’s just the canary in the coal mine. You think your heart’s fine because you’re not having a heart attack? Nah. Your eyes are already crumbling. Wake up.
Per the Keith-Wagener-Barker classification, Grade 2 retinal arteriolar narrowing with AV nicking demonstrates a statistically significant correlation (p<0.01) with microvascular endothelial dysfunction. The 22% prevalence rate in Stage 1 HTN aligns with longitudinal cohort data from the Atherosclerosis Risk in Communities Study. Early detection via OCT is now validated to detect retinal nerve fiber layer thinning prior to clinical symptoms.
So let me get this straight… the government doesn’t want you to know your eyes are dying from salt and stress… but they *do* want you to pay $300 for an ‘AI retinal scan’? 😏 Big Pharma’s new favorite accessory: the fundus camera. Next they’ll sell you ‘hypertension aura’ crystals. #WakeUpSheeple 🌈👁️
You people are out here treating your BP like it’s a suggestion. Bro, I had a cousin who ignored his numbers for 12 years - woke up one morning with a black spot in his vision. Turns out his retina was shredded like old pizza crust. He’s lucky he didn’t lose his sight or have a stroke. You think you’re fine because you don’t feel dizzy? That’s the whole damn point - you don’t feel it until it’s too late. Get your eyes checked. Now. Not tomorrow. TODAY.
Wait - so if I’m on an ACE inhibitor and my BP’s under 130/80, does that mean my retina’s actually healing? I had a scan last year and they said Grade 1, but I’ve been eating clean and taking my meds. Just want to know if it’s worth getting another scan this year… or if I’m just being paranoid 😅
It’s not just about your eyes - it’s about your soul. You let your blood pressure climb, you let your diet rot, you let your life become a series of pills and screens. And now you’re surprised your vision’s fading? You’ve been slowly murdering yourself with convenience. The retina doesn’t lie. It reflects the rot inside. If you can’t fix your habits, you don’t deserve to see clearly. Stop blaming the system. Start fixing yourself.
Okay but let’s be real - this whole ‘retinal damage’ thing is just a distraction. They’re using ‘hypertensive retinopathy’ to make you paranoid so you’ll keep buying meds and getting expensive scans. Meanwhile, the real cause? EMF radiation from your phone, 5G towers, and the fluoride in your water. My aunt in Kerala got her vision back after drinking neem water and avoiding WiFi. You think the FDA wants you to know that? No. They want you dependent. The retina is a spiritual antenna - when your energy is low, it dims. No doctor can fix that. Only consciousness can.
The elegance of this condition lies in its universality. It is not merely a medical phenomenon but a profound metaphor for systemic neglect - of the body, of the mind, of the social fabric that enables healthy living. The retina, as a direct extension of the central nervous system, mirrors the cumulative toll of chronic stress, poor nutrition, and systemic inequity in healthcare access. In societies where preventive care is inaccessible, hypertensive retinopathy becomes not just a disease, but a social indictment. The solution, therefore, must transcend pharmacology and extend into policy, education, and community-based health initiatives. We must treat the vessel, yes - but also the world that breaks it.
My grandma in Texas had this. Didn’t know until she couldn’t read her Bible. Got her BP under control, saw an eye doc every 6 months - now she’s 89 and still knitting. Point is: it’s not doom. It’s a nudge. Listen to the nudge.
I’m from Kenya - we don’t have OCT machines in most villages. But our healers have always said: ‘If your eyes are dim, your blood is thick.’ I’ve seen elders with hypertension who walk miles to get papaya leaves and hibiscus tea. They don’t have ACE inhibitors, but they live longer than most Americans. Maybe the answer isn’t just tech… maybe it’s tradition, rhythm, and food that remembers its roots.