Weight Loss Estimator Calculator
Estimate Your Weight Loss
How It Works
Based on clinical trial data from the article: Semaglutide typically produces 5-15% weight loss, while Tirzepatide shows 11.6-20%+ results. Your actual results may vary based on individual factors and adherence.
Estimated Weight Loss:
Important Considerations
- Note Weight loss results are estimates and may vary significantly
- Drug effects are dose-dependent (higher doses = greater results)
- Results typically stabilize after 6-12 months
- Weight maintenance requires continued medication
For years, diabetes medications were seen as tools to control blood sugar. But something unexpected happened: people using them started losing significant weight-sometimes 10%, 15%, even 20% of their body weight. That wasn’t an accident. It was built into the medicine. Today, GLP-1 agonists aren’t just for diabetes. They’re becoming the most effective weight loss tools we’ve ever had, and their benefits go far beyond the scale.
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a natural hormone your body makes after eating. That hormone, glucagon-like peptide-1, tells your pancreas to release insulin only when blood sugar is high. That’s smart design-it doesn’t crash your sugar levels like older diabetes drugs. But that’s not all it does. It also slows down how fast food leaves your stomach. And it talks directly to your brain, reducing hunger and making you feel full longer.
Think of it like this: your stomach sends a signal saying, ‘I’m full,’ but your brain ignores it. GLP-1 agonists turn up the volume on that signal. People on these drugs don’t just eat less-they stop craving high-calorie foods. A Reddit user on r/semaglutide described it as ‘the cravings just vanished. I didn’t even think about chips or cookies anymore.’
It’s not magic. It’s biology. And it works. In clinical trials, tirzepatide (Mounjaro, Zepbound) led to an average of 11.6% weight loss in people with type 2 diabetes. For those without diabetes but with obesity, some lost over 20% of their body weight. That’s not a few pounds. That’s 30, 40, even 60 pounds off for many.
Weight Loss That Outperforms Diet and Exercise Alone
People often think weight loss is just about eating less and moving more. And yes, those things matter. But when you compare lifestyle changes alone to lifestyle changes plus a GLP-1 agonist, the difference is staggering.
In the STEP-1 trial, people using semaglutide (Wegovy) along with diet and exercise lost nearly 15% of their body weight. The group that only did diet and exercise lost 2.4%. That’s a six-fold difference. And it wasn’t just temporary. Most kept the weight off for at least a year.
Compare that to older diabetes drugs. Sulfonylureas and insulin? They make you gain weight-often 4 to 10 kilograms on average. GLP-1 agonists are the opposite. They help you lose weight while keeping your blood sugar stable. That’s why the American Diabetes Association now recommends them as a first-line treatment for people with type 2 diabetes who also have obesity or heart disease.
Cardiovascular Benefits You Didn’t Know About
It’s not just about weight. People using GLP-1 agonists have a 12% to 18% lower risk of major heart events like heart attacks and strokes. That’s not a side effect-it’s a core benefit. Dr. Eric Polley’s 2024 study in Nature Cardiovascular Research found these drugs also reduced overall death risk by 8% to 14% in people with moderate heart disease risk.
That’s why drugs like Ozempic and Victoza got FDA approval specifically to lower heart risk in diabetic patients with existing heart disease. This isn’t a bonus. It’s a life-saving feature. For someone with diabetes and high blood pressure, a GLP-1 agonist isn’t just helping with their weight-it’s protecting their heart.

More Than Weight: The Hidden Benefits
Here’s where it gets even more surprising. In a 2024 study of over 2 million U.S. veterans, researchers found people on GLP-1 agonists had:
- 23% fewer seizures
- 17% lower risk of substance addiction (alcohol, opioids, cannabis, stimulants)
- 14% lower rates of suicidal thoughts
- 11% lower incidence of psychotic disorders like schizophrenia
- 16% fewer cases of bulimia
These weren’t just correlations. The study controlled for age, sex, income, and other health conditions. The link held. Experts still don’t fully understand why, but it’s likely tied to how GLP-1 receptors are found in the brain-areas that control mood, reward, and impulse. This could open the door to using these drugs for addiction treatment or depression down the line.
Side Effects: The Real Cost of Results
Nothing works without trade-offs. The biggest problem? Your stomach. About 30% to 50% of people get nausea, vomiting, or diarrhea-especially when starting. Most get better after a few weeks, but for some, it’s a dealbreaker.
One user on Drugs.com said, ‘Constant nausea made it hard to focus at work.’ Another reported, ‘I had to drop the dose because I couldn’t keep anything down.’
Then there’s ‘Ozempic face.’ It’s not a medical term, but it’s real. Long-term users report losing facial fat, making cheeks look hollow, skin looser. Harvard Health documented this in 42% of people who lost 20% or more of their body weight. It’s not dangerous, but it’s noticeable-and not always welcome.
There’s also a small risk of pancreatitis (0.5% to 1%) and gallbladder issues. These aren’t common, but they’re serious enough that doctors screen for them before prescribing.
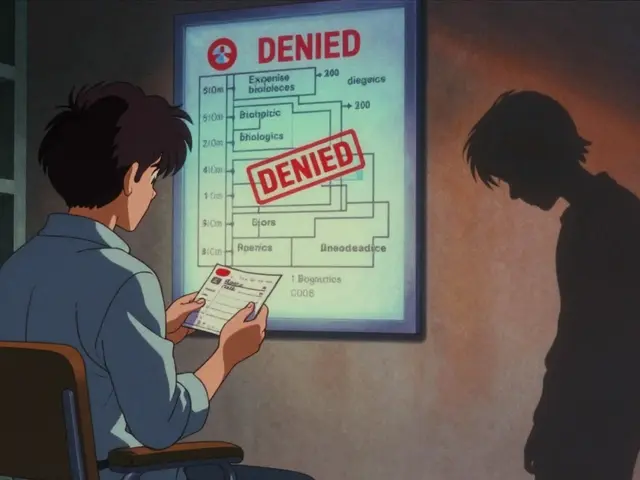
Cost and Access: The Biggest Barrier
Wegovy costs about $1,349 a month without insurance. Zepbound isn’t much cheaper. Most insurance plans won’t cover it unless you have diabetes or severe obesity. Even then, prior authorizations are a nightmare.
According to a 2024 survey, 58% of users struggled with insurance denials. Some people cut their doses in half to make it last longer. Others stop entirely when they can’t afford it. And when they stop? Weight comes back-fast. Studies show 50% to 70% of the weight returns within a year of quitting.
There are assistance programs. Novo Nordisk’s Norditrac covers up to 75% of out-of-pocket costs for eligible patients. Telehealth services like Found and Calibrate bundle the drug with coaching and nutrition-$99 to $149 a month on top of the medication. But for many, it’s still out of reach.
Who It Works For (and Who It Doesn’t)
GLP-1 agonists shine in people with:
- Type 2 diabetes and obesity
- Prediabetes and excess weight
- Heart disease and overweight
- Obesity without diabetes (Zepbound is FDA-approved for this)
But they’re not magic pills for everyone. In lean people without metabolic issues, the weight loss is minimal-and the side effects still happen. There’s no benefit to forcing it. And if you’re not willing to take it long-term, it’s not worth starting.
Dr. M. Rao, writing in American Family Physician, warns that weight cycling-losing and regaining-can raise blood pressure, trigger eating disorders, and even increase death risk. These drugs aren’t a quick fix. They’re a long-term tool.
The Future: What’s Next?
The market for these drugs exploded. Global sales hit $35.7 billion in 2023. By 2030, analysts predict they’ll hit $100 billion. Why? Because the need is huge. Nearly half of U.S. adults have obesity. Yet only 2% of eligible people are on these drugs.
Newer versions are coming. Oral semaglutide at higher doses (50 mg) is in Phase 3 trials. Triple agonists that target GLP-1, GIP, and glucagon are in development. Some companies are even testing 6-month implants.
Companies like Amazon and Walmart are adding GLP-1 agonists to employee health plans. Insurance coverage will likely improve as more data comes in. But until then, access remains unequal.
And the science keeps evolving. Researchers are now looking at whether these drugs can treat non-alcoholic fatty liver disease (NASH), Alzheimer’s, and even Parkinson’s. Early animal studies show promise. Human trials are just beginning.
How to Use Them Right
If you’re considering a GLP-1 agonist:
- Start low. Most doctors begin with 0.25 mg weekly (semaglutide) and slowly increase over 16 to 20 weeks to reduce nausea.
- Don’t skip meals. Eat protein-rich, fiber-filled meals. Low-carb diets often help manage side effects.
- Stay hydrated. Dehydration makes nausea worse.
- Use a support system. Online communities, nutritionists, and telehealth programs help people stick with it.
- Plan for the long haul. This isn’t a 3-month fix. It’s a lifestyle tool. If you stop, you’ll likely regain weight.
And always work with a doctor. These aren’t over-the-counter supplements. They require monitoring. Blood sugar, kidney function, and thyroid markers need checking.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, drugs like Wegovy and Zepbound are now FDA-approved specifically for chronic weight management in adults with obesity or overweight-regardless of whether they have diabetes. In fact, most prescriptions today are written for weight loss, not diabetes.
How much weight can I expect to lose?
Most people lose 5% to 15% of their body weight. With tirzepatide, some lose over 20%. Results vary based on dose, starting weight, diet, and activity level. The highest doses (like 2.4 mg semaglutide or 15 mg tirzepatide) produce the most weight loss, but also carry higher risk of side effects.
How long do I need to take them?
These drugs work only as long as you take them. Weight typically returns within a year of stopping. Experts now see them as long-term treatments, similar to blood pressure or cholesterol meds. You don’t stop after you reach your goal-you keep going to maintain it.
Is it safe to use GLP-1 agonists if I don’t have diabetes?
Yes, if you have obesity or overweight and meet FDA criteria. Zepbound and Wegovy are approved specifically for weight loss in people without diabetes. But you still need a doctor’s evaluation to rule out risks like thyroid tumors (in those with family history of medullary thyroid cancer) or pancreatitis.
Why do some people lose weight faster than others?
Genetics, metabolism, starting weight, diet, activity level, and how quickly your body adjusts to the drug all play a role. People with higher insulin resistance or more visceral fat often see faster results. Those who pair the drug with protein-rich meals and regular movement also tend to lose more and keep it off longer.




9 Comments
I started on semaglutide last year and honestly? My cravings just... disappeared. Not like I’m on some magic diet-I still eat pizza sometimes-but I don’t *need* it anymore. The nausea was rough at first, but after 3 weeks it faded. Now I’m down 22 lbs and my blood sugar’s never been better.
Oh great. So now we’re medicalizing laziness? Next thing you know, they’ll prescribe these to people who don’t want to get off the couch. I’ve seen this movie before-remember fen-phen? This is just pharma’s new cash cow dressed up as a miracle.
Chuck, I get your skepticism, but this isn’t about laziness. I’m a nurse who’s seen patients lose 60 pounds and finally walk without knee pain. These drugs don’t erase effort-they make it possible. The real tragedy is that people who need this can’t afford it. That’s not a flaw in the science. That’s a flaw in our system.
Marjorie’s right. I was on insulin for years and gained 30 lbs. Then I switched to semaglutide. Lost 40 lbs in 8 months. My A1C dropped from 8.2 to 5.7. And yeah, I still had to eat better and move-but now I *wanted* to. It’s not a pill that does all the work. It’s a tool that gives you the mental space to actually do the work. That’s huge.
Let’s not sugarcoat this-GLP-1 agonists are the most significant advance in metabolic medicine since metformin. But here’s the kicker: they’re not just weight-loss drugs. They’re neuroprotective, anti-inflammatory, appetite-modulating, reward-pathway-resetting agents. The fact that they reduce seizures, addiction risk, and suicidal ideation? That’s not a side effect-that’s a paradigm shift. We’re talking about drugs that don’t just treat symptoms but rewire the biological drivers of chronic disease. And yes, the cost is insane, and the ‘Ozempic face’ is real-but if you’re losing 20% of your body weight and cutting your heart attack risk by 18%, you’re not just surviving-you’re reclaiming your biology. This isn’t a trend. It’s a revolution.
It’s funny how everyone acts like this is the first time medicine has ‘solved’ obesity. It’s not. It’s just the first time Big Pharma found a way to monetize biology. The brain doesn’t crave cookies because it’s broken-it’s because we’ve engineered food to hijack it. These drugs suppress the symptom, not the cause. And now we’re turning people into lifelong drug-dependent patients for a condition we could prevent with policy, education, and food reform. We’re treating the symptom, not the system. That’s not progress. That’s capitulation.
So… I’m supposed to be impressed that a drug makes me not want chips? Cool. My dog doesn’t eat chips either. He’s just not human.
Given the data from the 2-million-veteran study, the reduction in substance use disorders and psychiatric events is statistically significant (p<0.001) and clinically meaningful, especially considering the controlled variables. The mechanism likely involves GLP-1 receptor expression in the nucleus accumbens and prefrontal cortex, which modulates dopamine signaling. This suggests potential for repurposing in addiction psychiatry-but long-term safety data beyond five years remains limited. I urge caution against over-enthusiasm until Phase 4 trials are published.
Let’s be real: this is just another way for rich people to buy their way out of consequences. Meanwhile, people without insurance are told to ‘eat less and move more’-but if they could, they wouldn’t need a $1,300 shot. This isn’t medicine. It’s a class war disguised as science. And now we’re normalizing it as ‘progress’? Wake up.