Probiotic-Antibiotic Timing Calculator
Enter your antibiotic dosage times below. This will help determine the optimal window for taking probiotics.
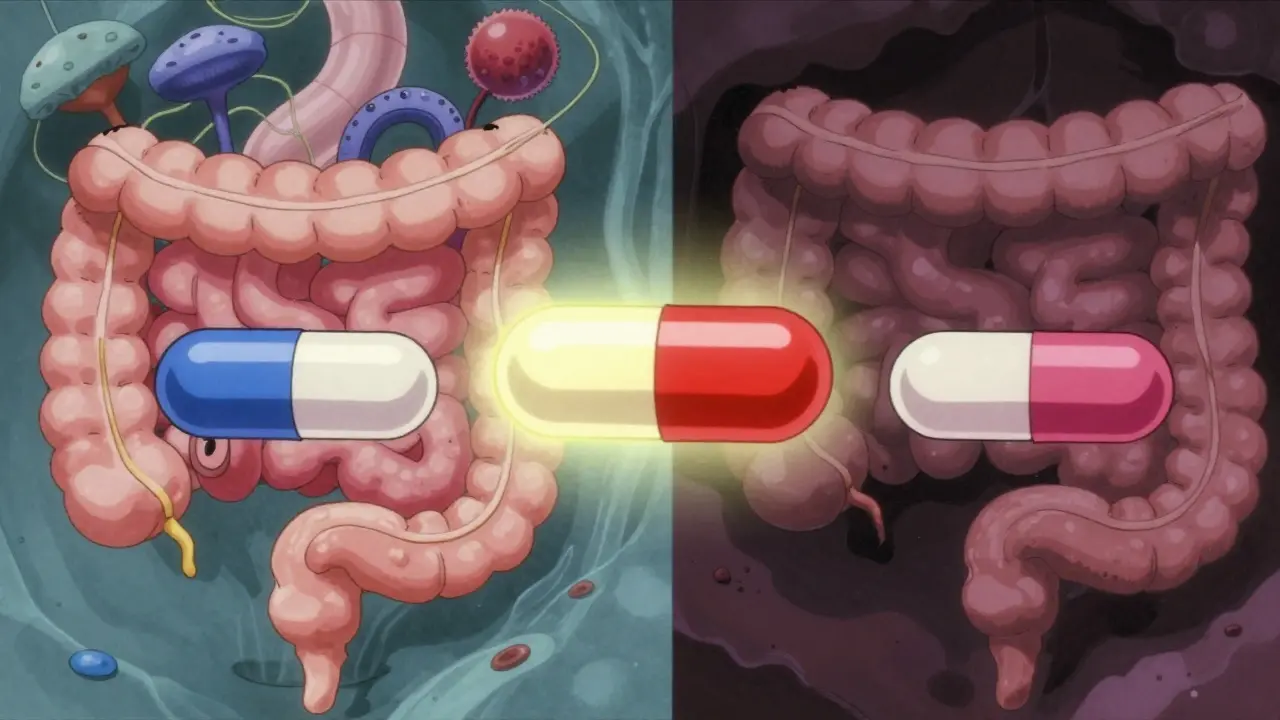
Antibiotics kill probiotic bacteria if taken at the same time. The recommended timing is at least 2 hours before or after your antibiotic dose. This allows probiotics to survive and begin repopulating your gut.
1. Enter your antibiotic dosing schedule
2. Click 'Calculate Optimal Timing'
3. Review the recommended probiotic timing
4. Take your probiotic during the recommended window to maximize effectiveness
The timeline below shows your antibiotic doses (blue) and recommended probiotic timing windows (green).
When you're on antibiotics, your gut pays the price. Even if the medicine kills off the bad bacteria causing your infection, it doesn’t care about the good ones keeping your digestion smooth. That’s why so many people end up with bloating, cramps, or worse - diarrhea that lasts days after finishing their pills. It’s not just discomfort. It’s your microbiome being wiped clean, like a hard drive reset with no backup.
That’s where probiotics come in. But here’s the catch: when you take them matters just as much as which ones you choose. Take them at the wrong time, and you might not help at all - or even slow down your gut’s natural recovery. Take them right, and you could cut your risk of antibiotic-associated diarrhea by nearly half.
Why Antibiotics Mess Up Your Gut
Antibiotics aren’t picky. They don’t know the difference between the bacteria causing your sinus infection and the ones helping you digest food. A typical course - say, amoxicillin or doxycycline - can knock out up to 90% of your gut bacteria in just a few days. Some of those microbes bounce back quickly. Others? They’re gone for months, sometimes years.
Studies show that even after you stop the antibiotics, your gut doesn’t return to normal right away. One 2018 study in Nature Microbiology found that people who took antibiotics took 132 extra days to get their native bacteria back compared to those who didn’t use probiotics. That’s almost four and a half months of imbalance. And during that time, you’re more vulnerable to infections, bloating, and even mood swings - because your gut and brain are deeply connected.
Do Probiotics Actually Help?
The answer isn’t simple. Some doctors swear by them. Others say they delay healing. Both sides have solid research behind them.
On one hand, a 2022 systematic review by the Microbiology Society found that taking probiotics alongside antibiotics reduced the risk of antibiotic-associated diarrhea by 48%. That’s not small. In fact, it’s one of the strongest effects you’ll see in any supplement study. The strains behind that number? Lactobacillus rhamnosus GG and Saccharomyces boulardii. These aren’t random bugs. They’ve been tested in over 20 clinical trials and consistently outperform other strains.
But here’s the twist. A 2024 study in Frontiers in Microbiomes showed something else: probiotics didn’t help restore the original gut bacteria any faster. In fact, people who took probiotics during antibiotics had slower recovery of their native microbes than those who didn’t. The probiotics were still alive, still active - but they were occupying space that your own bacteria needed to reclaim.
So you’re not choosing between good and bad. You’re choosing between two trade-offs: fewer side effects now, or slower long-term recovery.
When to Take Probiotics (The 2-Hour Rule)
If you decide to use probiotics, timing is everything. The most consistent advice from Harvard Medical School, the Cleveland Clinic, and the American Gastroenterological Association is this: take your probiotic at least 2 hours before or after your antibiotic dose.
Why? Because antibiotics can kill probiotic bacteria if they’re in your system at the same time. If you take them together, you’re essentially feeding your antibiotic a snack of good bacteria - and it will eat them.
Most people find it easiest to take probiotics at bedtime, right before sleep. That’s because antibiotics are usually taken in the morning and evening. A bedtime dose gives you a 6-8 hour gap from the last antibiotic, reducing the chance of interference.
Some users report better results taking probiotics 2 hours before the antibiotic - especially if they’re on a once-daily dose. Others prefer right after the antibiotic, but that’s riskier. Stick to the 2-hour window. It’s not magic, but it’s the most proven buffer.
Which Strains Actually Work?
Not all probiotics are created equal. There are over 500 commercial strains on the market. Only five have strong evidence for reducing antibiotic diarrhea.
- Lactobacillus rhamnosus GG - The most studied. Reduces diarrhea risk by 26% compared to multi-strain blends.
- Saccharomyces boulardii - A yeast, not a bacteria. Works even when antibiotics are still active. Especially helpful for people on clindamycin or broad-spectrum drugs.
- Lactobacillus plantarum 299v - Less known but promising. One study showed 37% better preservation of gut diversity than other strains.
- Bifidobacterium lactis - Helps with bloating and gas, common side effects of both antibiotics and probiotics.
- Streptococcus thermophilus - Often paired with other strains. Helps break down lactose, which can be hard to digest after antibiotics.
Multi-strain products? They sound better, but they’re not. The 2022 Cochrane review found single-strain formulas - especially GG and S. boulardii - worked better than blends. Stick to one or two proven strains.

How Much Should You Take?
Dosage matters. Too little, and you won’t see results. Too much, and you might feel worse.
Most studies use between 5 billion and 40 billion CFU (colony-forming units) per day. For most healthy adults, 10-20 billion CFU is enough. If you’re older, have a weakened immune system, or are on a long or strong antibiotic (like vancomycin), go with 20-40 billion CFU - but talk to your doctor first.
Storage is another hidden factor. Strains like L. rhamnosus GG and S. boulardii need refrigeration. If your bottle sits on the counter for weeks, half the bugs may be dead. Look for products labeled "refrigerated" or check the expiration date. Shelf-stable probiotics? They’re convenient, but often less effective.
What About Food Sources?
You don’t need pills. Yogurt, kefir, sauerkraut, kimchi, miso, and kombucha all contain live cultures. But here’s the problem: they don’t have enough bugs.
A typical serving of yogurt might have 1-2 billion CFU. That’s not enough to compete with antibiotics. Plus, the strains in fermented foods aren’t always the ones proven to help with antibiotic side effects.
Food is great for long-term gut health. But during antibiotic treatment, supplements give you the targeted, high-dose punch you need.
Who Should Avoid Probiotics?
Most people can take them safely. But not everyone.
If you’re immunocompromised - say, you’re on chemotherapy, have HIV, or had an organ transplant - probiotics can cause serious infections. There are documented cases of bloodstream infections from probiotic bacteria in vulnerable people.
Also, if you’ve had recent surgery, especially involving your gut, or if you have a central IV line, skip them. The risk, though rare, is real.
And if you’re already bloated or gassy? Probiotics can make it worse - temporarily. Some strains produce gas as they work. That’s normal. But if it lasts more than 3-4 days, stop and talk to your doctor.
The Bottom Line: What to Do
Here’s what works, based on real studies and expert consensus:
- Choose Lactobacillus rhamnosus GG or Saccharomyces boulardii - they’re the most reliable.
- Take 10-20 billion CFU daily. Go up to 40 billion if you’re high-risk or on strong antibiotics.
- Take your probiotic 2 hours before or after your antibiotic. Bedtime is easiest.
- Keep it refrigerated. Check the expiration date.
- Keep taking it for 1-2 weeks after your antibiotic ends. Some experts recommend up to 4 weeks for broad-spectrum drugs.
- Stop if you have severe bloating, fever, or signs of infection.
It’s not a guarantee. But it’s your best shot at avoiding the worst side effects without making your gut recovery worse.
What the Experts Disagree On
Dr. Elisa Marroquin says probiotics protect your gut during antibiotics. Dr. Martin Blaser says they delay recovery. Both are right - depending on what you’re measuring.
If your goal is to avoid diarrhea, probiotics win. If your goal is to get your original gut bacteria back as fast as possible, they might slow you down. That’s why there’s no universal rule.
The science is still evolving. A 2025 study in Nature found people on probiotics during antibiotics reported better mood after two weeks - suggesting a link to the gut-brain axis. But we still don’t know if that’s from the probiotics themselves or just from avoiding diarrhea and sleepless nights.
For now, go with what works for you: fewer stomach issues, even if it takes a little longer for your gut to fully heal.
What’s Next?
Researchers are now testing personalized probiotic timing - matching strains to your gut type, antibiotic, and even your diet. The International Scientific Association for Probiotics and Prebiotics just launched a $4.2 million project to standardize this research.
But you don’t need to wait. Right now, with the right strain and timing, you can take control of your gut health during antibiotics. No guesswork. No fluff. Just science-backed steps.
Antibiotics saved your life. Don’t let your gut pay the price.


9 Comments
So you’re telling me I’ve been taking probiotics WITH my antibiotics this whole time?? Like, right after my amoxicillin?? 😭 I’ve been suffering from diarrhea for WEEKS-now I know why. I’m not even mad, just… devastated. This post just saved my colon. I’m switching to bedtime probiotics tomorrow. No more mistakes. I swear on my gut.
Bro, this is gold! 🙌 I’m from India, and we’ve been drinking buttermilk and eating curd after antibiotics for generations-but no one ever told us about the 2-hour rule! Now I get why my uncle still gets bloated even after probiotics. I’m sharing this with my whole family. And yes, L. rhamnosus GG is the one I’ll grab. Thanks for the clarity, man!
Just finished a 10-day course of doxycycline and took probiotics daily at bedtime-no diarrhea, no bloating. I used Renew Life’s GG strain (20 billion CFU). Refrigerated. Exp date checked. I didn’t feel like a lab rat. I just felt… normal. This works. Don’t overcomplicate it.
While the empirical evidence supporting the 2-hour separation protocol is robust, it is imperative to acknowledge the methodological heterogeneity across the cited studies. For instance, the 2024 Frontiers in Microbiomes paper employed a non-randomized cohort design, which may introduce selection bias. Furthermore, the definition of "native microbiome recovery" varied substantially between cohorts. A meta-analysis of double-blind, placebo-controlled trials would yield more definitive conclusions.
Wait so S. boulardii is a yeast? That’s wild. I always thought probiotics were just bacteria. I’ve been taking that one for my mom after her chemo-she’s got a central line though… should I stop? I don’t wanna risk it. Anyone know if it’s safe for chemo patients? I’ll check with her oncologist but just wanted to see if anyone’s tried it.
This is exactly the kind of clear, science-backed advice we need more of. No hype, no fluff. Just facts. I’ve been recommending this to my patients for years but never had such a concise guide to share. Thank you for taking the time to lay this out so thoughtfully. Your work matters.
The paradox of probiotic intervention lies not in its efficacy per se, but in the ontological assumption that microbial colonization is synonymous with health. The human microbiome is not a static ecosystem to be restored, but a dynamic, context-dependent network. To introduce exogenous strains during antibiotic perturbation may, in fact, represent a form of ecological interference-however well-intentioned. Perhaps the true remedy is not supplementation, but the removal of the conditions that necessitate antibiotics in the first place.
So let me get this straight… we’re supposed to take expensive, refrigerated pills to avoid diarrhea… but the real solution is just not taking antibiotics unless absolutely necessary? 😏 Funny how the whole industry sells us the band-aid instead of fixing the wound.
Probiotics are a Big Pharma scam to sell you more pills. The real reason you get diarrhea after antibiotics is because the government added fluoride to the water to kill your gut bugs so they can track your emotions through your bowels. They’ve been doing this since 2012. The CDC won’t tell you. But I found the leaked memo. Check the expiration date on your probiotic? That’s not for freshness. That’s the kill switch. Don’t trust any of this. I’m not even taking my antibiotics anymore.