
Medication-Induced Nosebleed Risk Calculator
Assess Your Nosebleed Risk
Select medications you're currently taking to see your risk level and get prevention tips.
Select your medications to see your risk level
Important Note: This tool provides general guidance only. Never stop prescribed medications without consulting your doctor.
Why Your Nose Bleeds When You Take Common Medications
It’s not just dry air or a bad habit of picking your nose. If you’ve been getting frequent nosebleeds and you’re on any kind of regular medication, there’s a good chance the two are connected. Nosebleeds - or epistaxis - happen to about 60% of people at some point in their lives. But for those taking certain drugs, the risk jumps significantly. You might not think of ibuprofen or aspirin as culprits, but they’re among the top offenders. So is warfarin, clopidogrel, even over-the-counter nasal sprays if used too long.
The real issue isn’t that these drugs are dangerous. They’re often life-saving. But they interfere with how your body stops bleeding. Some thin your blood. Others dry out the inside of your nose. Either way, the tiny blood vessels in your nasal lining become easy targets. And when they pop, you bleed - sometimes for minutes, sometimes for longer.
Which Medications Are Most Likely to Cause Nosebleeds?
Not all meds cause nosebleeds the same way. There are three main groups to watch for:
- NSAIDs - These include ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. Even low-dose aspirin (81 mg), taken daily to protect your heart, can reduce your blood’s ability to clot. A single dose can be enough to trigger bleeding in someone with already sensitive nasal vessels.
- Blood thinners - Warfarin (Coumadin), clopidogrel (Plavix), and heparin are designed to prevent clots, but that means they also make bleeding harder to stop. People on these drugs are far more likely to have nosebleeds that last longer or come back often. Heparin can even cause a rare but serious reaction called HIT, which leads to both clotting and bleeding problems.
- Nasal decongestants and antihistamines - Sprays like oxymetazoline (Afrin) shrink blood vessels in your nose to clear congestion. But if you use them for more than 3 days, your nose rebounds - the vessels swell back even bigger, and the lining dries out. This makes it fragile and prone to cracking and bleeding.
Acetaminophen (Tylenol) is the rare exception. It doesn’t affect clotting like NSAIDs do, which is why doctors often recommend it for pain or fever if you’re prone to nosebleeds.
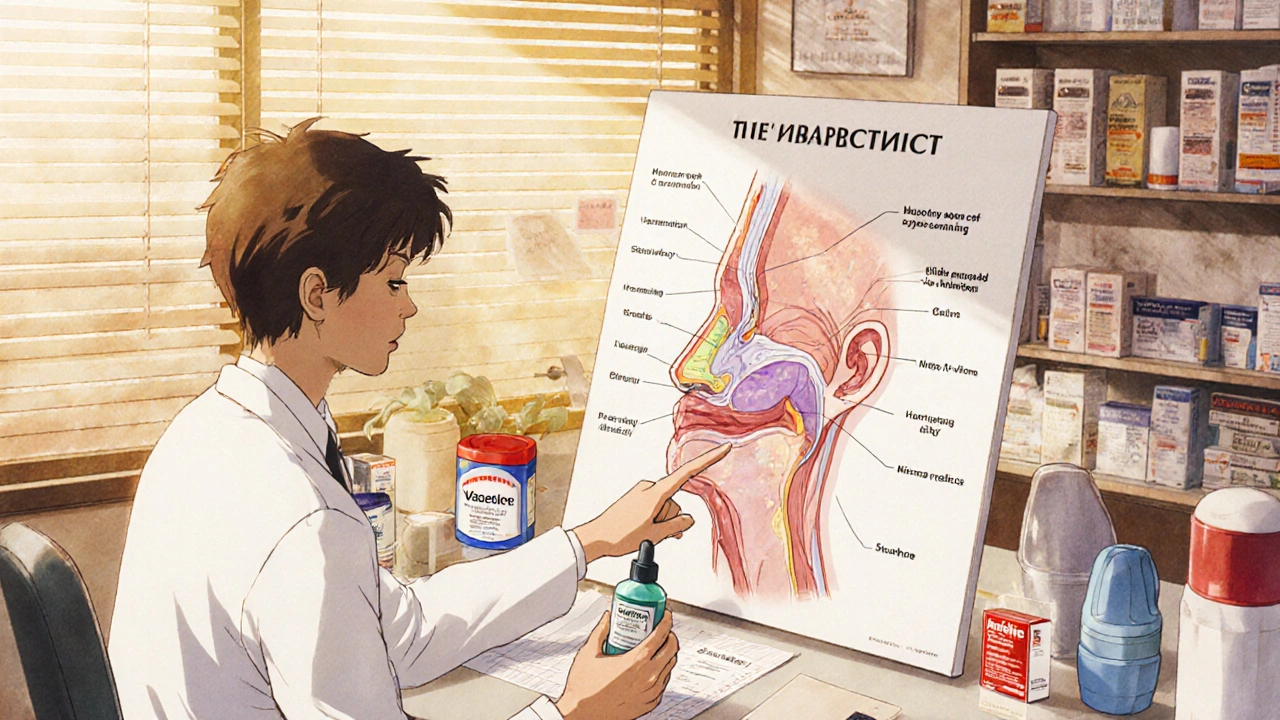
Why Your Nose Is So Vulnerable
Your nose isn’t just a passageway for air. Inside, there’s a dense network of tiny blood vessels called Kiesselbach’s plexus. It’s one of the most vascular areas in your body - perfect for warming and humidifying air, but also easy to damage. When medications weaken the lining or thin your blood, this area becomes a weak spot.
Think of it like paper. Normal nasal tissue is like thick cardstock. NSAIDs and blood thinners make it feel like tissue paper. Decongestants dry it out until it’s brittle. A little bump - even from blowing your nose too hard - can cause a tear. And because the vessels are so close to the surface, they bleed fast and often.
Children are especially at risk. They pick their noses, have thinner nasal linings, and are more likely to be on common cold meds. Older adults (45-80) face higher risk too - their vessels are more fragile, and they’re more likely to be on multiple medications. Pregnant people also see changes: blood volume increases, vessels expand, and nasal tissues swell. Add a medication on top, and the risk goes up again.
How to Prevent Medication-Related Nosebleeds
Stopping your meds isn’t the answer - unless your doctor says so. Instead, focus on protecting your nose.
- Moisturize daily - Apply a thin layer of petroleum jelly (Vaseline) inside each nostril, twice a day - morning and before bed. Saline nasal sprays or gels work too. Keep the inside of your nose soft and slick.
- Use a humidifier - Dry indoor air, especially in winter, is a major trigger. A cool-mist humidifier in your bedroom helps keep nasal membranes hydrated. Aim for humidity above 40%.
- Avoid nose picking and rubbing - This is the #1 thing you can do to prevent trauma. Keep nails short. If you feel itchy, use a saline spray instead.
- Limit decongestant sprays - Never use oxymetazoline or similar sprays for more than 3 days in a row. They’re great for short-term relief, but they set you up for worse problems later.
- Switch pain relievers - If you’re taking ibuprofen or aspirin regularly and getting nosebleeds, ask your doctor about switching to acetaminophen. It’s just as effective for pain and fever, and doesn’t affect clotting.
What to Do When You Get a Nosebleed
Most nosebleeds stop on their own - if you handle them right.
- Pinch your nose - Use your thumb and index finger to squeeze the soft part of your nose shut. Don’t just press on the bridge - you need to compress the vessels inside. Hold for 10-15 minutes. Set a timer. Most people give up too soon.
- Stay upright and lean forward - Tilting your head back sounds natural, but it makes you swallow blood. That can cause nausea, vomiting, or even choking. Lean forward slightly and breathe through your mouth.
- Don’t blow your nose - Wait at least 12 hours after the bleeding stops. Blowing can reopen the wound.
- Use a decongestant spray only if needed - If the bleeding doesn’t stop after 10 minutes, you can spray one puff of oxymetazoline into the bleeding nostril. It shrinks blood vessels fast. But don’t use it regularly - just as a one-time helper.
When to Call a Doctor
Not every nosebleed needs medical care. But these signs mean it’s time to get help:
- Bleeding lasts longer than 20 minutes, even with pressure
- You feel dizzy, lightheaded, or faint
- You’re coughing up or vomiting blood
- You’re bruising easily or bleeding from other places (gums, urine, stool)
- You’ve had a recent head or facial injury
- You’re on blood thinners and the nosebleed won’t stop
- You’re getting more than 3-4 nosebleeds in a week
If you’re on warfarin, your doctor may check your INR (a blood test that measures clotting time). If it’s too high, they might adjust your dose or give you vitamin K to reverse the effect. For those on newer blood thinners like apixaban or rivaroxaban, there are specific reversal agents available in emergencies.
Work With Your Pharmacist and Doctor
You don’t have to figure this out alone. Pharmacists are trained to spot drug interactions and side effects. Tell them you’re getting nosebleeds. They can review all your meds - including supplements and OTC drugs - and flag any that might be contributing.
Your doctor can also help you weigh the risks. Yes, aspirin might be causing nosebleeds. But if you’re taking it to prevent a heart attack or stroke, stopping it could be more dangerous than the bleeding. The goal isn’t to eliminate all meds - it’s to manage the risk. That might mean switching one drug, adding nasal moisturizers, or adjusting dosages.
For patients with chronic nosebleeds and complex medication regimens, specialists sometimes use nasal cautery or balloon catheters to seal off problem vessels. But those are last-resort options. Most cases improve with simple changes to your daily routine and medication habits.
Final Thought: It’s Not Just a Minor Annoyance
Nosebleeds from medication might seem small - until they’re not. For someone on blood thinners, even a minor bleed can become serious fast. For kids, frequent nosebleeds can mean missed school or anxiety. For older adults, it can signal a bigger problem with clotting or high blood pressure.
The good news? You can almost always reduce or prevent these bleeds without stopping your essential medications. It’s about understanding how your body reacts, protecting your nasal lining, and communicating with your care team. A little moisture, a few smart swaps, and some patience go a long way.
Can over-the-counter cold medicine cause nosebleeds?
Yes. Many OTC cold and allergy medicines contain decongestants like pseudoephedrine or oxymetazoline. These shrink blood vessels in the nose, but overuse leads to rebound swelling and dryness, making the lining fragile. Antihistamines like diphenhydramine can also dry out nasal tissues. Use these only as directed and for short periods - no more than 3 days in a row.
Is it safe to take aspirin daily if I get nosebleeds?
If you’re taking low-dose aspirin (81 mg) for heart protection, don’t stop it without talking to your doctor. The risk of a heart attack or stroke usually outweighs the risk of nosebleeds. But you can reduce the bleeding by using saline sprays, humidifiers, and avoiding nose picking. Ask your doctor if switching to acetaminophen for pain relief is an option.
Do blood thinners always cause nosebleeds?
No. Not everyone on warfarin, Plavix, or similar drugs gets nosebleeds. But your risk is higher than average. Factors like dry air, nose picking, high blood pressure, or using NSAIDs at the same time can increase the chance. Regular moisturizing and avoiding trauma are key to preventing them.
Can nasal saline sprays make nosebleeds worse?
No. In fact, they’re one of the best ways to prevent them. Saline sprays keep the inside of your nose moist, which helps protect the blood vessels. Use them 2-3 times a day, especially in dry weather or if you’re on decongestants or antihistamines. Avoid sprays with additives - plain saline is best.
Should I stop my medication if I start getting nosebleeds?
Never stop a prescribed medication on your own. Many of the drugs that cause nosebleeds - like blood thinners or aspirin - are critical for your health. Instead, talk to your doctor or pharmacist. They can help you figure out if the nosebleeds are linked to your meds, and if there’s a safer alternative or a way to reduce the risk without stopping treatment.





17 Comments
I used to get nosebleeds every week until I started using Vaseline at night. No more drama. Just a tiny dab inside each nostril. Game changer.
Also stopped taking ibuprofen for headaches. Went to tylenol and boom-no more blood.
Simple stuff, but nobody talks about it.
Let me tell you something that no one else will admit-this entire medical system is built on profit-driven pharmaceutical propaganda. You think aspirin is for your heart? No. It’s for the stockholders of Pfizer and Merck. They know damn well it dries out your nasal mucosa and makes you dependent on their saline sprays and humidifiers. They profit from your bleeding. They profit from your fear. They profit from your ignorance. And now you’re just another consumer scrubbing your nostrils with petroleum jelly like a peasant in a medieval plague village. Wake up. The system is rigged. You’re not just getting nosebleeds-you’re being monetized.
The pathophysiology here is well-documented: NSAIDs inhibit COX-1, reducing thromboxane A2 synthesis in platelets, which impairs primary hemostasis. In the Kiesselbach’s plexus, where vascular density is exceptionally high and epithelial integrity is mechanically fragile, this creates a perfect storm for capillary rupture. Add xerotic mucosal changes from decongestant rebound, and you’ve got a iatrogenic epistaxis triad. The solution isn’t avoidance-it’s mitigation. Moisturization, humidity control, and strategic analgesic substitution are evidence-based. No mysticism required.
Y’all are overthinking this 💀
Stop taking the poison. Stop picking your nose. Put Vaseline on it. Done.
Why are we still having this conversation in 2025? We have apps that tell us when to pee. But we can’t figure out not to use Afrin for 10 days straight? Come on. 🤦♂️
This is such a helpful breakdown. I’ve been on Plavix for my stent and had nosebleeds every other week. Started the petroleum jelly routine and a humidifier-no more bleeding. Honestly, I felt like a failure until I read this. You’re not broken. Your nose just needs a little TLC. You got this.
I must point out a critical oversight in the original post: the failure to address the potential role of hypertension in exacerbating epistaxis in patients on anticoagulants. While pharmacologic interference is indeed a primary contributor, uncontrolled systolic blood pressure above 140 mmHg significantly increases vascular shear stress, thereby compounding the risk of mucosal rupture. This comorbidity must be evaluated concurrently. Furthermore, the omission of any mention of tranexamic acid nasal sprays-a topical antifibrinolytic with proven efficacy in recurrent epistaxis-is scientifically indefensible.
I want to say thank you to whoever wrote this. As a nurse who’s seen patients come in with nosebleeds so bad they needed cauterization, I can tell you-this is the kind of info that saves lives. And I especially appreciate the part about not stopping meds without talking to your doctor. So many people just quit their blood thinners because they’re scared. That’s way more dangerous than the bleed. You’re not alone. Talk to your pharmacist. Use the saline. Put the jelly on. It’s not weak. It’s smart. And you’re doing better than you think.
Okay but if you’re taking aspirin daily and you’re getting nosebleeds, you’re basically asking for it. I mean, come on. You think your heart is more important than your nose? You’re 65, on 10 meds, and still using Afrin like it’s candy. That’s not a medical issue-that’s a lifestyle issue. Stop being lazy and start taking care of yourself. I’m not being mean. I’m being real.
I’ve been reading this article for 20 minutes and I’m still not sure if I’m supposed to be scared or relieved. I take warfarin. I use Afrin. I pick my nose. I don’t use humidifiers. I’ve had 7 nosebleeds this month. I think I’m dying. I think I’m a bad person. I think I’m going to bleed out in my sleep. I think I need to move to a rainforest. I think I need a new doctor. I think I need to call my mom. I think I need to stop reading Reddit. I think I need to lie down.
Simple. Moisturize. Stop picking. Talk to doc. Done.
Did you know that the FDA approved nasal sprays with oxymetazoline without long-term safety studies? And that the same companies that make these sprays also fund the 'heart health' campaigns pushing daily aspirin? It’s not coincidence. It’s control. They want you dependent. They want you bleeding. They want you coming back for more. Look at the numbers-nosebleed ER visits spiked 200% after the 2010 aspirin guidelines. Coincidence? I think not.
We are all just dust trying to hold together. The nosebleed? Just the universe reminding us we’re temporary. 🤍
But also-yes, use Vaseline. And stop taking ibuprofen like it’s candy. Your body isn’t a machine. It’s a poem. And poems need softness.
I used to think nosebleeds were just a thing that happened to old people. Then I started taking melatonin for sleep and got one every morning. Turns out, melatonin can thin blood too. No one tells you that. Not even the label. So I stopped. And now I’m fine. But I still don’t trust any supplement. Or doctors. Or labels. Or anything really.
Man, I love how this post doesn’t just dump facts-it gives you a roadmap. Like, ‘here’s the problem, here’s why it sucks, here’s how to fix it without losing your life-saving meds.’ That’s rare. I’ve been using the Vaseline trick for 3 months now. My wife thinks I’m weird for doing it before bed, but my nose hasn’t bled since. And honestly? I feel like a wizard now. I’ve got my little jar of magic jelly. 🧙♂️
Wait so… acetaminophen doesn’t cause nosebleeds? 😳 I’ve been taking Advil for my migraines for years. I think I just found my new go-to. Thank you!! 💕
In many South Asian cultures, we use rosewater or aloe vera gel to soothe nasal dryness. It’s traditional, gentle, and effective. I’ve used it for years alongside my blood pressure meds. No bleeding. No drama. Just cool, calm moisture. Maybe it’s worth exploring beyond petroleum jelly. Natural doesn’t mean unscientific.
I tried rosewater once. Felt nice. But Vaseline sticks better. Still works.