When you need a strong topical steroid, Clobetasol is often prescribed for stubborn skin conditions. It’s a high‑potency, prescription‑only corticosteroid that can calm inflammation in psoriasis, eczema, and certain rashes, but it also carries a set of risks if not used correctly. Knowing how to discuss it with your doctor can make the difference between a successful treatment and unwanted side effects.
Why a Conversation Matters
Doctors balance the benefits of rapid symptom relief against the potential for skin thinning, hormonal effects, and allergic reactions. By asking the right questions, you help them tailor the dosage, duration, and monitoring plan to your unique situation.
7 Tips for a Productive Talk
- Do Your Homework - Look up clobetasol’s potency level (it’s classified as Class I, the strongest category) and common side effects. A basic understanding shows you’re engaged and makes the doctor’s explanations clearer.
- Bring Your Medical History - Prepare a list of past skin issues, previous steroid use, allergies, and any systemic medications. This helps the doctor decide whether clobetasol is safe for you.
- Ask About Alternatives - Inquire whether a lower‑potency steroid (like betamethasone) or a non‑steroidal option could work. Knowing the trade‑offs lets you weigh effectiveness against risk.
- Clarify Application Details - Request exact instructions: how much to apply, how often, and whether to use a finger‑tip amount or a specific amount per square inch. Misapplication is a common cause of side effects.
- Set a Timeline - Ask how long you should stay on clobetasol and what signs indicate it’s time to stop. Most guidelines recommend a short course (2‑4 weeks) for localized areas.
- Discuss Monitoring - Request a follow‑up plan. Will the doctor check skin thickness, check blood sugar, or ask about new symptoms? Regular check‑ins catch problems early.
- Know the Red Flags - Ask which symptoms (e.g., severe burning, spreading rash, sudden weight gain) warrant an immediate call or visit.
Key Takeaways
- Clobetasol is a high‑potency corticosteroid; use only as directed.
- Bring a concise medical history and list of current meds.
- Ask about dosage, application area, and treatment duration.
- Set a clear follow‑up schedule to monitor side effects.
- Know the warning signs that require urgent medical attention.

Comparing Common Topical Steroids
| Steroid | Potency Class | Typical Indications | Typical Duration |
|---|---|---|---|
| Clobetasol | Class I (Super‑high) | Psoriasis, severe eczema, lichenoid eruptions | 2‑4 weeks (short‑term) |
| Betamethasone | Class II‑III (High‑moderate) | Moderate eczema, dermatitis, insect bites | 4‑6 weeks |
| Hydrocortisone | Class VII (Low) | Mild rash, allergic reactions, sunburn | As needed, up to several weeks |
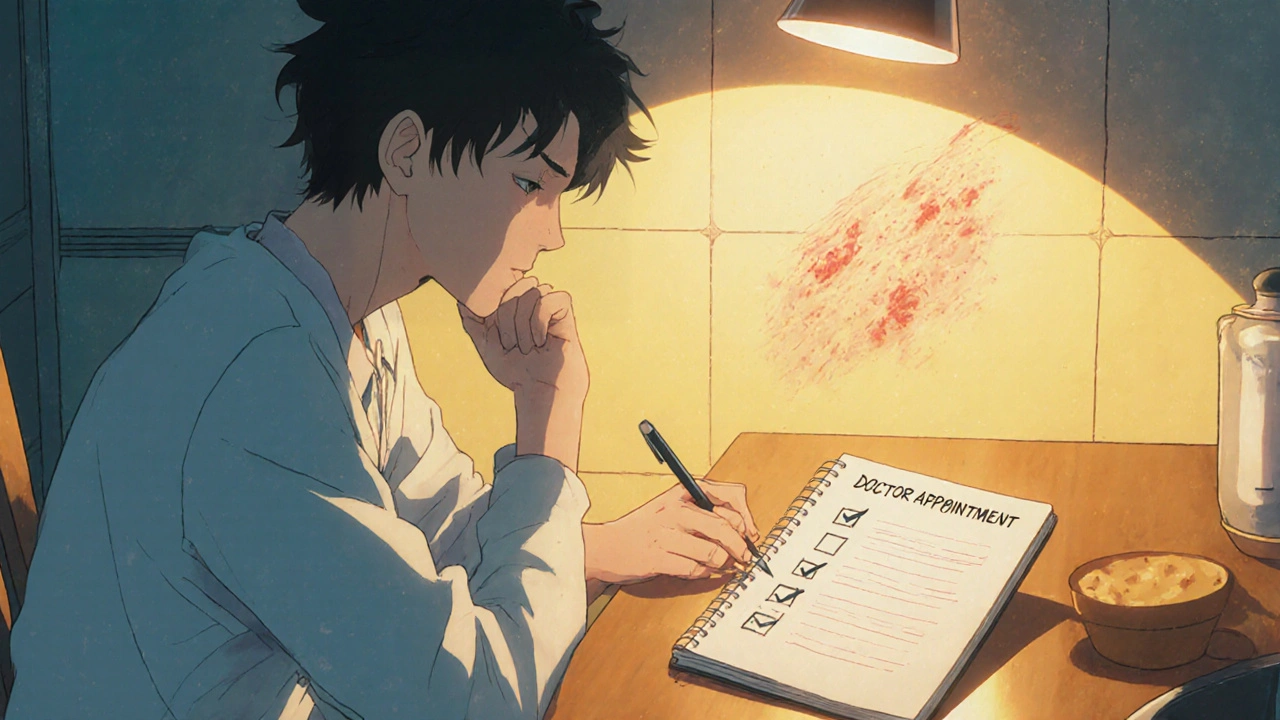
How to Prepare for Your Appointment
Write down the following points the night before:
- The specific skin area that’s bothering you (size, location, duration).
- Any over‑the‑counter creams you’ve already tried.
- All known drug allergies (especially to steroids or preservatives).
- Recent changes in weight, blood pressure, or blood sugar - systemic steroids can affect these.
Bring the list to the exam room. A concise note keeps the conversation focused and shows respect for the clinician’s time.
Understanding Prescription Details
When the doctor writes clobetasol, the prescription will include:
- Strength - Usually 0.05% cream or ointment.
- Quantity - How many grams or tubes you should receive.
- Directions for Use - “Apply a thin layer to the affected area twice daily for 14 days.”
- Refill Instructions - Often “No refills unless re‑evaluated.”
If any part of the label is unclear, ask the pharmacist to repeat it. Ambiguity is a common source of misuse.

When to Seek Immediate Help
Even though clobetasol is effective, it can cause serious problems if it spreads to larger skin areas or is used on broken skin. Call your doctor (or go to the emergency department) if you notice:
- Intense burning or stinging that doesn’t fade after a few minutes.
- Rapidly spreading redness or swelling.
- Signs of infection: pus, warmth, fever.
- Unexplained weight gain, facial swelling, or mood changes - possible systemic absorption.
Wrapping Up the Conversation
Before you leave, repeat back the plan in your own words. This “teach‑back” method confirms you’ve understood the dosage, duration, and warning signs. Write the key points on a piece of paper or note them in your phone.
Frequently Asked Questions
Can I use clobetasol on my face?
Because the facial skin is thin, clobetasol is generally avoided on the face except under close supervision for severe conditions like discoid lupus. Your dermatologist may prescribe a lower‑potency steroid instead.
How long is it safe to stay on clobetasol?
Most guidelines recommend no more than 2‑4 weeks for a single area. If you need longer treatment, your doctor will likely cycle off the drug and monitor skin thickness.
What should I do if I miss a dose?
Apply the missed dose as soon as you remember, then continue with the regular schedule. Avoid doubling up, as that increases the risk of side effects.
Are there any drug interactions I should worry about?
Topical clobetasol has minimal systemic interaction, but if you’re using oral steroids, immunosuppressants, or certain antifungal creams, discuss it with your physician to avoid additive effects.
Can I use clobetasol while pregnant or nursing?
Data are limited, but short‑term, limited‑area use is generally considered low risk. Always inform your OB‑GYN and dermatologist before starting treatment.
Approaching the appointment with clear goals, a concise medical background, and the right questions turns a potentially complicated prescription into a manageable, effective plan. When you bring up clobetasol confidently, you empower both yourself and your doctor to achieve the best skin‑health outcome.





9 Comments
Got the lowdown on clobetasol potency it’s Class I super‑high high‑potent topical steroid works fast but watch skin thinning.
First, it’s great that you’re taking charge of your clobetasol therapy. Understanding the potency class helps you gauge the risk‑benefit balance. You should always mention any past steroid use so the dermatologist can adjust the dose appropriately. A clear medication list, including over‑the‑counter creams, prevents accidental interactions. When discussing alternatives, ask about mid‑potency options like betamethasone; sometimes they’re sufficient and carry fewer side effects. Be specific about the application amount – a fingertip unit for each affected area is a common guideline. Ask how often you should apply it and whether you need to space the doses. Setting a clear treatment timeline, such as a two‑week course, reduces the chance of overuse. Request a follow‑up appointment to monitor skin thickness and check for systemic effects. If you notice any burning, worsening rash, or signs of infection, call your doctor right away. Inquire about the red‑flag symptoms like unexplained weight gain or facial swelling. Make sure you understand the refill policy – most prescribers will want a reassessment before renewing. Write down the directions in your own words before leaving the office; the teach‑back method is a proven way to confirm comprehension. Keep a small journal of how your skin responds each day, noting any irritation or improvement. Finally, don’t hesitate to bring up any concerns about pregnancy, breastfeeding, or other health conditions, as adjustments may be necessary.
Wow, this guide really hits the mark, doesn’t it? I love how it breaks down each step, from homework to red‑flags, and it feels super approachable! The tip about “teach‑back” is pure gold, because repeating the plan in your own words locks it in memory. Also, the reminder to bring a concise medical history saves both you and the doctor time – win‑win! If you ever feel nervous, just breathe and remember the doctor wants you to be informed. Keep the checklist handy, and you’ll walk into the appointment like a pro!
Thanks for the rundown, will add it to my notes.
They don’t want you to know that pharma pushes clobetasol as a quick fix while they collect data on skin thinning across the population.
Don’t waste your time with half‑measures.
Oh great, another “must‑read” post about a steroid that only dermatologists understand. Because we all have endless spare minutes to memorize potency classes, right? Maybe next time they’ll write a novel on how to apply a cream without breaking the universe.
Keep it simple, stick to the basics, and you’ll be fine.
Look, you’ve got the info, the checklist, the doctor’s questions – there’s no excuse to skip the follow‑up. If you ignore the red flags, you’re basically signing up for preventable damage, and that’s just not cool.