Every year, over 100,000 people in the U.S. die from drug overdoses. Most of those deaths involve synthetic opioids like fentanyl - a drug so powerful that even a tiny amount can stop someone’s breathing in under a minute. If someone in your home takes prescription pain medication, you’re not just a caregiver - you could be their best chance at survival. The truth? Overdose doesn’t always look like a dramatic scene from a TV show. Sometimes, it looks like a person sleeping too deeply. That’s why having a clear, practiced plan isn’t optional. It’s lifesaving.
Why Your Family Needs This Plan
You don’t need to be a doctor to save a life. You just need to know what to do - and act fast. The window between when someone stops breathing and when brain damage begins is only 4 to 6 minutes. Emergency services can take 7 to 12 minutes to arrive. That’s why the person next to them matters more than anyone else.Studies show that when naloxone (the overdose reversal drug) is given within those first few minutes, it works over 90% of the time. But only 12% of households with prescription opioids have a plan in place. That means most families are flying blind. This isn’t about fear. It’s about preparedness - like having a fire extinguisher or a first aid kit.
Step 1: Know Which Medications Are in Your Home
Start by listing every medication in the house that could cause an overdose. This includes:- Opioid painkillers (oxycodone, hydrocodone, fentanyl patches, morphine)
- Sedatives (benzodiazepines like Xanax or Valium)
- Medications for sleep or anxiety
- Any drug prescribed for chronic pain
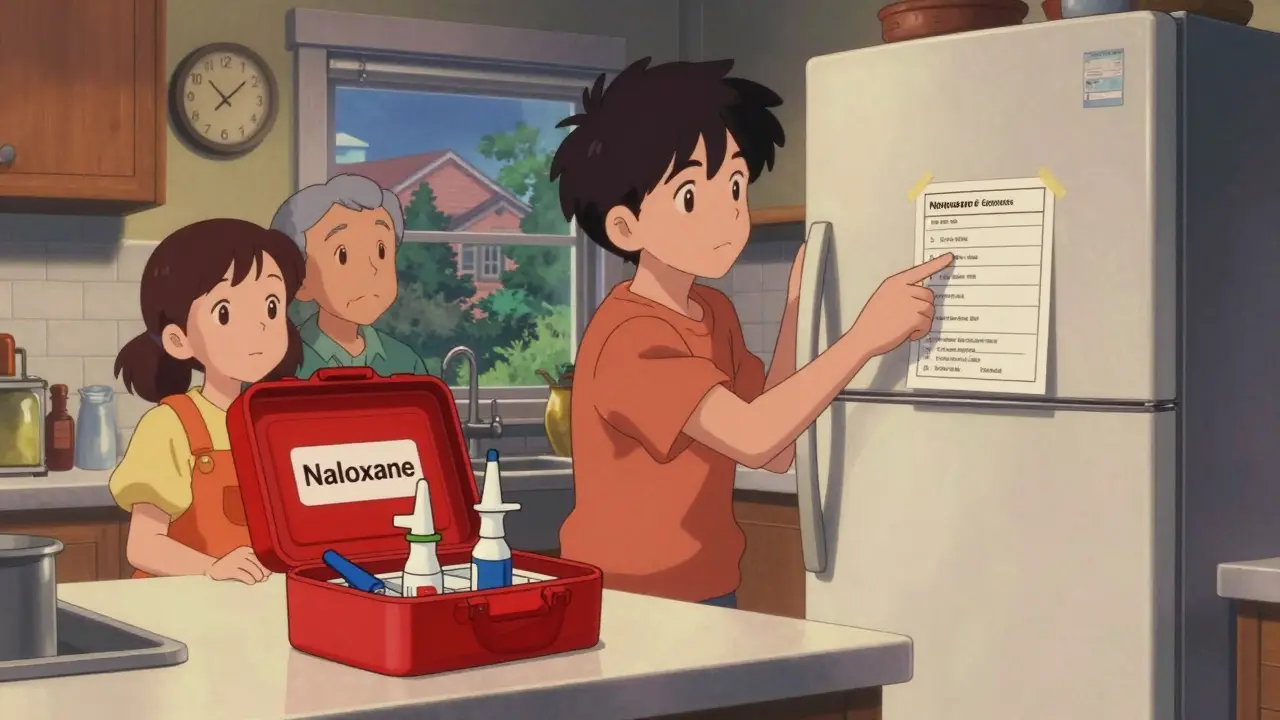
Write down the name, dosage, prescribing doctor, and how often it’s taken. Keep this list on a laminated card in your wallet or taped to the fridge. If someone overdoses, first responders need this info fast. It tells them what they’re dealing with - and whether they’ll need more than one dose of naloxone.
Step 2: Get Naloxone - And Know How to Use It
Naloxone (brand names Narcan or Kloxxado) is the only drug that can reverse an opioid overdose. It’s safe, non-addictive, and works even if the person didn’t take opioids - it won’t hurt someone who didn’t overdose.Here’s how to get it:
- Most pharmacies in Canada and the U.S. sell it without a prescription
- Many pharmacies offer it for $25 or less with insurance
- Free kits are available through public health clinics, community centers, and some hospitals
Keep at least two doses on hand. Fentanyl and other synthetic opioids are so strong that one dose of naloxone might not be enough. Store them at room temperature (between 68°F and 77°F), away from direct sunlight. Check the expiration date every 18 months. If it expires, replace it - don’t wait.
Step 3: Learn the Signs of Overdose
An overdose doesn’t always mean someone is slumped over. Look for these three signs:- Unresponsive: Shake their shoulder hard. Call their name. If they don’t wake up, it’s an emergency.
- Abnormal breathing: Are they gasping? Snoring? Or not breathing at all? Normal breathing is 12-20 breaths per minute. Less than 12 is dangerous.
- Pinpoint pupils: Shine a flashlight in their eye. If the pupils are tiny dots, that’s a red flag.
If you see even one of these signs - especially with a known opioid user - assume it’s an overdose. Don’t wait for all three.

Step 4: Practice the Emergency Response
Every member of your household - including teens - should know what to do. Use the A.N.C.H.O.R. method:- Assess: Check for responsiveness and breathing.
- Naloxone: Administer one dose of naloxone immediately. For nasal spray, insert the nozzle into one nostril and press the plunger fully. For injection, give it into the thigh muscle through clothing if needed.
- Call 911: Dial emergency services right after giving naloxone. Say: “I gave naloxone for a possible opioid overdose.”
- Have more ready: Keep the second dose nearby. If they don’t wake up in 3-5 minutes, give the second dose.
- Observe: Stay with them. Even if they wake up, they can relapse into overdose. Keep monitoring for at least 2 hours.
- Review: After the event, talk as a family. What worked? What was confusing? Update your plan.
Practice this sequence every few months. Use a toy or a dummy to simulate giving the nasal spray. Muscle memory saves lives.
Step 5: Make It Visible and Accessible
Don’t hide naloxone in a locked cabinet. If someone’s overdosing, you won’t have time to search. Keep it in a bright, labeled container - like a red box on the kitchen counter or next to the bathroom sink. Teach everyone where it is.Also, leave a printed copy of your emergency plan near the phone, on the fridge, and in your phone’s notes. Include:
- Your address
- Emergency contacts
- Names and dosages of all medications
- How to use naloxone (with a QR code linking to a video if possible)
One family in Halifax told us they kept their plan inside a waterproof case taped to the back of their medicine cabinet. When their son overdosed, his 15-year-old sister found it in under 10 seconds. She gave the naloxone. He woke up. EMS arrived 8 minutes later. He’s alive today because of that plan.
What About Non-Opioid Overdoses?
Naloxone only works on opioids. If someone overdoses on alcohol, benzodiazepines, or other drugs, naloxone won’t help. But calling 911 still does. In those cases:- Don’t give them coffee or cold showers - those don’t work
- Keep them on their side to prevent choking
- Stay with them until help arrives
Some families mix opioids with alcohol or sleep aids. That’s a dangerous combo. If that’s happening in your home, talk to a doctor. There are safer alternatives.

Common Mistakes and How to Avoid Them
- “I thought they were just sleeping.” - Don’t wait. If they don’t respond to a shoulder shake, act.
- “The naloxone expired.” - Check dates every 18 months. Replace it.
- “I was scared to call 911.” - Good Samaritan laws protect you in all 50 U.S. states and Canadian provinces. You won’t get in trouble for calling.
- “I didn’t know how to use it.” - Watch a 5-minute video on YouTube or ask your pharmacist to show you. Practice once a month.
What Happens After the Overdose?
Even if naloxone works, the person isn’t “out of the woods.” The effects of naloxone wear off after 30-90 minutes. But opioids - especially fentanyl - can stay in the body for hours. That means they can stop breathing again. That’s called renarcotization.That’s why you must:
- Keep monitoring for at least 2 hours
- Never leave them alone
- Stay with them until EMS takes over
Afterward, many people who survive an overdose go into treatment. Studies show 89% of those who get naloxone help later seek counseling or rehab. This isn’t a failure. It’s a turning point.
Training and Resources
You don’t need a medical degree. Free training is available:- American Red Cross: 15-minute online course (available in English and French)
- Washington State DOH: Free in-person trainings
- Local public health units: Many offer free naloxone kits with training
- Project COPE (New York): Teaches the A.N.C.H.O.R. method
Some apps, like Overdose Guardian (released in January 2024), give real-time alerts if overdoses are happening near you. That helps you stay aware - not scared.
Final Thought: This Isn’t About Prediction. It’s About Protection.
You can’t predict who will overdose. But you can prepare for it. Every family with opioids in the house should treat naloxone like a fire extinguisher: you hope you never need it. But if you do, you’ll be glad you kept it handy.Start today. Talk to your family. Get the kit. Practice the steps. Update your list. It takes less than two hours - and it could save a life tomorrow.
Can I get naloxone without a prescription?
Yes. In all U.S. states and Canadian provinces, naloxone is available without a prescription at pharmacies. Many offer it for $25 or less with insurance. Some clinics give it away for free.
What if I give naloxone and the person doesn’t wake up?
Give a second dose after 3-5 minutes. Call 911 immediately. Even if they don’t respond, keep monitoring. Some overdoses require multiple doses, especially with fentanyl. Don’t stop until help arrives.
Is naloxone safe to use if I’m not sure it’s an overdose?
Yes. Naloxone has no effect on someone who hasn’t taken opioids. It won’t hurt them. If they’re unresponsive and not breathing normally, giving naloxone is the right move - even if you’re unsure.
Do I need to train everyone in the house?
Yes. Teens and children are often the first to find someone overdosing. Train everyone who lives in the home - even if they’re young. A 12-year-old can learn to use a nasal spray. Practice makes it automatic.
What if I’m afraid to talk about this with my family?
Start small. Say: “I’m worried about what would happen if someone had a bad reaction to their medicine. Let’s make a plan - just in case.” You’re not predicting tragedy. You’re building safety. Most families say they wish they’d done it sooner.


8 Comments
I never thought about this until my cousin OD’d last year. Turns out his fentanyl patch was leaking and he just looked like he was passed out. We had no plan. No naloxone. Just panic. Now I keep two doses on the fridge with a printed A.N.C.H.O.R. card taped to it. My sister’s 14 and she knows exactly what to do. Scary stuff, but way scarier not to be ready.
Also, stop calling it "drug abuse" - it’s not a moral failure. It’s a medical emergency. Treat it like one.
Naloxone should be as common as smoke detectors.
This is exactly the kind of performative safety theater that clogs up public health discourse. You don’t need a laminated card. You don’t need a red box. You need a society that stops prescribing opioids like candy in the first place. This plan treats symptoms, not the disease. The real solution? Defund the pharmaceutical lobby. Stop the marketing. Stop the overprescribing. Stop pretending that giving out nasal sprays is somehow progress.
I work in public health in Mumbai and I can tell you this plan is useless without context. In the U.S., you have pharmacies, insurance, and naloxone on shelves. In India, we don’t even have clean needles. You’re talking about a luxury solution for a problem that doesn’t even exist the same way here. Stop exporting your first-world panic as universal wisdom. Also, your "A.N.C.H.O.R." method? Sounds like a corporate buzzword. Real emergency responders don’t use acronyms - they use instinct and training. And no, your 12-year-old shouldn’t be responsible for saving your addict relative. That’s not empowerment - that’s child endangerment.
The universe speaks in quiet tragedies - a still chest, a silent phone, a medicine cabinet left unopened. We build walls of denial until the walls collapse. Naloxone isn’t a tool - it’s a whisper from the future saying: "You still have time."
I keep mine in a mason jar with a handwritten note: "For love, not fear." My daughter says it looks like a potion. I tell her it is. The potion of presence. The spell of staying. The incantation: "I am here. I see you. I will not look away."
And yes - I cry every time I check the expiration date. But I do it anyway. Because love isn’t passive. It’s a practice. A ritual. A second dose. A breath. A heartbeat. A choice.
I’ve seen this exact post before. It’s a feel-good PSA dressed up as a lifesaving guide. But let’s be real - if someone’s taking opioids this way, they’re already deep in addiction. You don’t save people like this with a laminated card. You save them with therapy, housing, and dignity. This plan just makes families feel like they’ve done their part. Meanwhile, the real system - the one that overprescribed, underfunded, and abandoned these people - keeps rolling. Stop pretending this is a fix. It’s a Band-Aid on a hemorrhage.
The A.N.C.H.O.R. method is a joke. First, you don’t "assess" - you act. If they’re unresponsive, you give naloxone. No time for checklists. Second, calling 911 after giving the dose? That’s backwards. Call 911 FIRST. Then give naloxone. Third, why are you telling people to keep it on the counter? What if a kid finds it? What if it’s stolen? You’re not helping - you’re creating liability. And don’t get me started on the "12-year-old can do it" nonsense. That’s not empowerment - that’s negligence wrapped in virtue signaling.
To everyone who’s dismissed this plan as performative or naive: I’ve trained over 300 families in rural Appalachia. I’ve held the hands of mothers who found their sons blue and silent. I’ve watched teens administer naloxone before EMS arrived. This isn’t about perfection. It’s about possibility. One dose. One life. One moment of courage. You don’t need a degree. You need a heart. And if you’re still arguing about systems instead of saving lives right now - then you’re not helping. You’re just talking. Let’s get the kits. Let’s practice. Let’s stop waiting for someone else to fix it. You are the system.