Beta-Blocker & Calcium Channel Blocker Safety Calculator
Patient Assessment
Enter key patient factors to determine safety of beta-blocker and calcium channel blocker combination therapy.
When doctors prescribe beta-blockers and calcium channel blockers together, it’s not random. It’s a calculated move-usually for patients with high blood pressure that won’t budge with one drug, or for those with angina and a fast heartbeat. But this combo isn’t safe for everyone. In fact, the difference between a life-saving treatment and a dangerous mistake often comes down to one thing: which type of calcium channel blocker you’re using.
How These Drugs Work Together
Beta-blockers like metoprolol and atenolol slow your heart rate and reduce the force of each heartbeat by blocking adrenaline. Calcium channel blockers like amlodipine and verapamil relax your blood vessels by keeping calcium out of heart and artery cells. On paper, they sound like a perfect team: one lowers heart rate, the other lowers pressure. Together, they can bring down blood pressure more effectively than either alone.
But here’s the catch-some calcium channel blockers don’t just relax blood vessels. They also slow down your heart’s electrical system. That’s where things get risky.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are the same. There are two main types, and mixing them with beta-blockers has wildly different outcomes.
Dihydropyridines-like amlodipine, nifedipine, and felodipine-mainly target blood vessels. They barely touch the heart’s rhythm. That’s why when paired with a beta-blocker, they’re generally safe. Studies show this combo reduces heart attacks and strokes in hypertensive patients without triggering dangerous drops in heart rate.
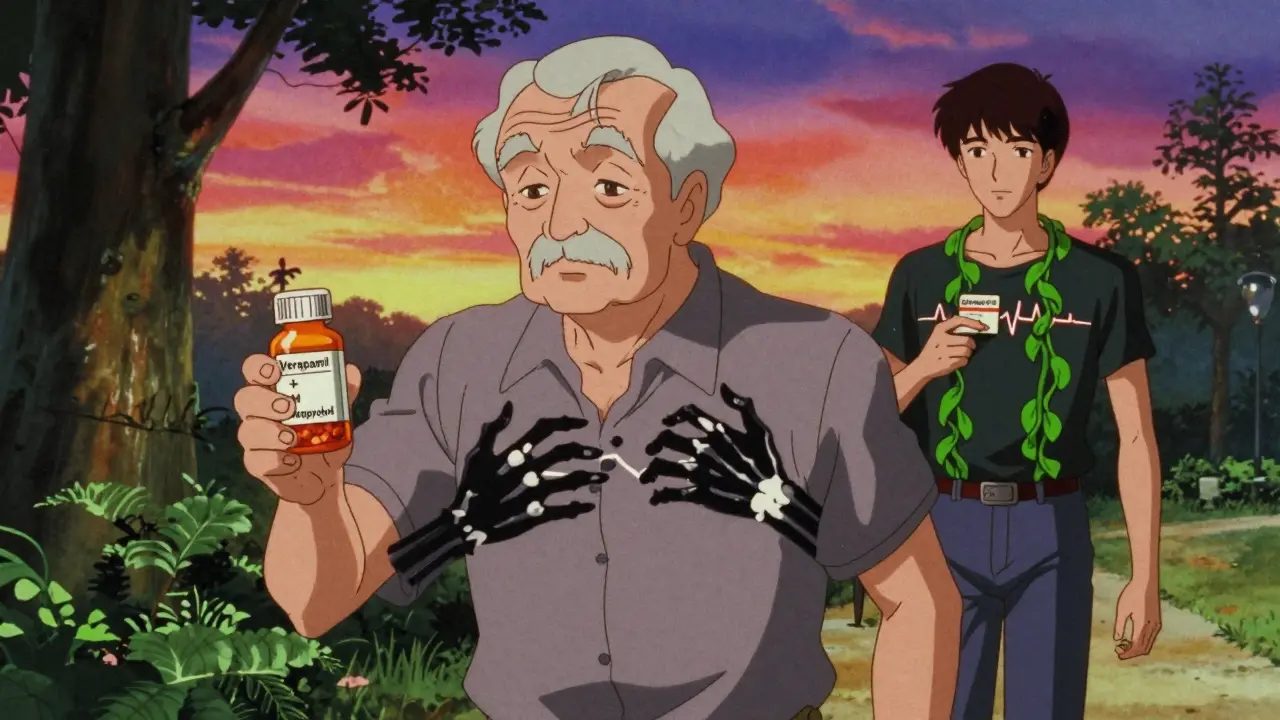
Non-dihydropyridines-verapamil and diltiazem-are different. They hit both the heart and the blood vessels. When you add them to a beta-blocker, you’re essentially double-dosing on heart slowdown. The result? A higher chance of bradycardia (heart rate below 50), heart block, or even heart failure in vulnerable patients.
A 2023 study of nearly 19,000 Chinese patients found that those on beta-blocker + verapamil had a 10-15% risk of needing emergency treatment for slow heart rhythms. That number dropped to under 3% with beta-blocker + amlodipine.
Who Should Avoid This Combo?
If you have any of these, beta-blocker + verapamil or diltiazem is a bad idea:
- Already slow heart rate (under 55 bpm at rest)
- PR interval longer than 200 milliseconds on ECG (a sign of delayed electrical signal in the heart)
- Second- or third-degree heart block
- Sinus node dysfunction (your heart’s natural pacemaker isn’t working right)
- Heart failure with reduced ejection fraction (EF under 45%)
Even if you don’t have these conditions, age matters. Patients over 65 are 3.2 times more likely to need a pacemaker after starting verapamil with a beta-blocker than those on amlodipine. That’s not a small risk-it’s a red flag.
What About Side Effects?
Even the safer combos come with trade-offs.
Swelling in the ankles-peripheral edema-is common with amlodipine. About 22% of patients get it, compared to 16% on other combos. It’s usually mild and can be fixed by lowering the dose. But if you’re already on a beta-blocker, your body can’t compensate as easily, so swelling might stick around longer.
Another issue: fatigue. Both drugs can make you feel tired. When combined, that feeling can double. Some patients stop taking them not because they’re dangerous, but because they just feel “dragged down.”
And then there’s the hidden danger: undiagnosed conduction problems. One in seven people over 75 has a slow heart rhythm they don’t know about. If you start verapamil without an ECG, you could trigger complete heart block-something that needs a pacemaker, fast.
When Is This Combo Actually Useful?
It’s not all risk. There are clear cases where this combo shines.
Angina with high heart rate-If you get chest pain when you’re active and your heart races to 100 bpm just climbing stairs, beta-blocker + amlodipine can help you walk farther without pain. One study showed patients improved exercise time by nearly two minutes.
Resistant hypertension-When three drugs haven’t lowered your pressure enough, adding amlodipine to a beta-blocker can be the final push. It’s especially helpful if you’re African American, have kidney disease, or are older.
Supraventricular arrhythmias-For people with atrial fibrillation or flutter, the combo can help control heart rate better than either drug alone. But again, only if you’re on amlodipine-not verapamil.

What Doctors Do Before Prescribing
Good clinicians don’t just write a script. They check three things first:
- ECG-to measure PR interval and look for hidden blocks
- Echocardiogram-to check ejection fraction and rule out heart failure
- Medication review-to spot other drugs that might worsen the combo (like digoxin or certain antidepressants)
Then they start low and go slow. A typical plan: begin with half the usual dose of each drug, wait a week, check heart rate and blood pressure, then adjust. Weekly check-ins for the first month are standard.
There’s even an online calculator from the European Society of Cardiology that estimates your risk of bradycardia based on age, kidney function, and baseline ECG. It’s 89% accurate.
What Patients Are Saying
On medical forums, stories vary wildly.
A cardiologist in Boston shared: “I’ve put over 200 patients on metoprolol + amlodipine. Only three had ankle swelling I couldn’t fix. No one had a slow heart rate that needed treatment.”
But on Reddit, a doctor wrote: “Lost a patient last month to complete heart block after adding verapamil to metoprolol. He was 82. PR was 210ms-barely above normal. I didn’t think it was enough to worry about. I was wrong.” That post got over 140 upvotes. Others echoed: “I avoid verapamil with BB in anyone over 70. Full stop.”
A 2022 survey of 1,247 U.S. doctors found 78% prefer beta-blocker + dihydropyridine combos. Only 12% would use verapamil, even in ideal cases. The top reason? Fear of bradycardia.
The Bottom Line
Beta-blockers and calcium channel blockers can work well together-but only if you pick the right one. Amlodipine? Safe and effective for most. Verapamil or diltiazem? Dangerous in many cases.
If you’re on this combo, ask your doctor: “Which type of calcium channel blocker am I on?” If it’s verapamil or diltiazem, and you’re over 65, have a slow pulse, or feel unusually tired, get an ECG. Don’t wait for symptoms to get worse.
Doctors aren’t ignoring the risks. Guidelines from Europe and the U.S. now say: avoid non-dihydropyridines with beta-blockers unless there’s no other option. And even then, only with close monitoring.
This isn’t about avoiding treatment. It’s about choosing the right one. The right combo can save your heart. The wrong one can stop it.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes, but only with the right type of calcium channel blocker. Beta-blockers paired with dihydropyridines like amlodipine are generally safe and effective for hypertension and angina. Combining them with non-dihydropyridines like verapamil or diltiazem can cause dangerous drops in heart rate or heart block, especially in older adults or those with existing heart rhythm issues.
What’s the biggest risk of combining beta-blockers and verapamil?
The biggest risk is severe bradycardia or heart block. Studies show 10-15% of patients on this combo develop slow heart rhythms that require emergency treatment. In patients over 65, the risk of needing a pacemaker is over three times higher than with amlodipine. This is why guidelines now warn against using verapamil with beta-blockers in most cases.
Why is amlodipine safer than verapamil with beta-blockers?
Amlodipine is a dihydropyridine calcium channel blocker that mainly relaxes blood vessels without significantly affecting the heart’s electrical system. Verapamil, a non-dihydropyridine, slows both heart rate and electrical conduction. When combined with a beta-blocker-which also slows the heart-the effects multiply, leading to dangerous heart rate drops. Amlodipine avoids this synergy.
Should I get an ECG before starting this combo?
Absolutely. Guidelines require a baseline ECG to check your PR interval and rule out hidden heart block. If your PR interval is over 200 milliseconds, you’re at high risk for dangerous slowing of the heart if you take verapamil or diltiazem with a beta-blocker. Even if you feel fine, an ECG can catch problems you don’t know you have.
What are the signs I should stop this medication?
Stop and call your doctor if you feel dizzy, faint, extremely tired, or notice your pulse dropping below 50 beats per minute. Shortness of breath, swelling in your legs, or chest pain could also signal worsening heart function. Don’t wait-these can be early signs of heart block or heart failure triggered by the combo.
Is this combo still used today?
Yes, but selectively. Beta-blocker + amlodipine is still commonly used for high blood pressure with angina or high resting heart rate. Beta-blocker + verapamil is now rarely prescribed and only in very specific cases under close supervision. Most doctors avoid it entirely after 2021 FDA warnings and 2022 clinical guidelines.


9 Comments
Man, I’ve been on amlodipine + metoprolol for 3 years. Ankle swelling? Yeah, but I just wear socks with sandals and call it a day. No dizziness, no fainting - just a guy who can now climb stairs without feeling like he’s running a marathon.
Let’s be real - this isn’t just about pharmacology. It’s about how medicine has become a game of risk minimization instead of patient empowerment. We’re so afraid of verapamil causing bradycardia that we’re ignoring the fact that untreated hypertension kills silently, daily, in living rooms and nursing homes alike. The real tragedy isn’t the combo - it’s the fear-driven inertia of modern prescribing. We optimize for liability, not life. And yes, I’ve seen patients on amlodipine who still end up in heart failure because we never addressed their insulin resistance, their sleep apnea, their chronic stress. This is a band-aid on a bullet wound, dressed up as science.
They don’t want you to know this, but verapamil was pulled from the market in Europe for a reason - big pharma pushed amlodipine because it’s cheaper to make and has no patent expiration. The ‘danger’ of verapamil? A distraction. They want you on lifelong meds, not cured. And don’t get me started on ECGs - why do you think they charge $800 for one? It’s not for your health. It’s for their profit margins. You think your doctor really cares? Nah. They’re paid by the pill, not by the pulse.
There is a statistically significant increase in the incidence of complete heart block when non-dihydropyridine calcium channel blockers are co-administered with beta-blockers in patients over the age of 65 with a PR interval exceeding 200 ms, as documented in the 2023 Chinese cohort study (n=18,942). The hazard ratio was 3.21 (95% CI: 2.78–3.72), p<0.001. Furthermore, peripheral edema incidence with amlodipine is not merely ‘mild’ - it is a dose-dependent, clinically relevant adverse effect that reduces adherence by up to 37% in elderly populations. The assertion that ‘no one had a slow heart rate that needed treatment’ is anecdotal and lacks longitudinal follow-up data. I recommend consulting the 2022 ESC guidelines on conduction system drug interactions for proper risk stratification.
They’re lying. All of them. The FDA didn’t issue warnings - they buried them. The same people who told you statins were safe for everyone are the ones now saying verapamil is deadly. Why? Because the pacemaker industry is worth $20 billion. They need you slow. They need you dependent. They need you scared. That ECG? It’s not to protect you - it’s to create a billing code. And that ‘online calculator’? Built by a hospital network that owns 14 cardiac clinics. You’re not being helped. You’re being monetized.
It’s funny how we treat medicine like a math equation - drug A + drug B = outcome C. But the human body isn’t a spreadsheet. It’s a living, breathing mess of emotions, sleep, trauma, gut bacteria, and unspoken grief. Maybe the fatigue isn’t from the meds - maybe it’s from working two jobs and never feeling seen. Maybe the slow pulse isn’t dangerous - maybe it’s your soul finally resting. I’m not saying skip the ECG. I’m saying ask yourself: who are you really healing? The heart? Or the system that made you feel broken in the first place?
I’ve been on metoprolol + amlodipine for 4 years. My BP’s down, my chest pain’s gone, and my ankles swell a little - but I walk 5 miles every morning anyway. I don’t see this as a risk vs. reward thing. I see it as a tool. You wouldn’t throw out a hammer because it can hit your thumb. You learn how to use it. The key isn’t avoiding the combo - it’s knowing your body, getting checked, and not letting fear make the call. My doc started me on half-dose, waited, adjusted. Simple. Human. No conspiracy. Just care.
Did you know that in 2021, the CDC quietly updated their guidelines to say that patients on beta-blockers should be screened for sleep apnea before adding any CCB? No one talks about this. Why? Because sleep apnea causes bradycardia too - and if you’re on verapamil AND have untreated sleep apnea, your heart can literally stop overnight. But insurance won’t pay for the sleep study unless your doctor codes it as ‘suspected arrhythmia’ - which requires an ECG first. So you’re stuck in a loop. They don’t want you to know. They want you to just take the pill.
Just got my ECG back - PR was 198ms. Doctor said I’m good to go on amlodipine. Felt like I just passed a life test. Thanks for this post - it made me ask the right questions. No panic, no fear. Just info. And that’s all I needed.